Cicatricial alopecia due to sarcoidosis
Published Web Location
https://doi.org/10.5070/D39pt7x94sMain Content
Cicatricial alopecia due to sarcoidosis
Thaer Douri, A Zahi Chawaf, Bdour Aboutouk Alrefaee
Dermatology Online Journal 9 (1): 16
Syria. s-dori@scs-net.org.Abstract
Sarcoidosis of the scalp is a rare manifestation of cutaneous sarcoidosis. We report a case in a Syrian man without systemic involvement. Sarcoidosis should be considered in the differential diagnosis of cicatricial and non-cicatricial alopecia along with discoid lupus erythematous (DLE), lichen planopilaris, and scleroderma.
Case Report
 |
| Figure 1 |
|---|
| Figure 1. Patchy hair loss with absence of follicles. |
A 32 year old Syrian man presented with a progressive patchy hair loss of 8 month's duration. The affected areas of the scalp were mildly pruritic. Treatment with topical corticosteroids was without benefit. Physical examination revealed two discrete, erythematous, round patches of cicatricial alopecia (Figure 1). The patient was healthy and a review of systems and past medical history were unrevealing.
 |
| Figure 2 |
|---|
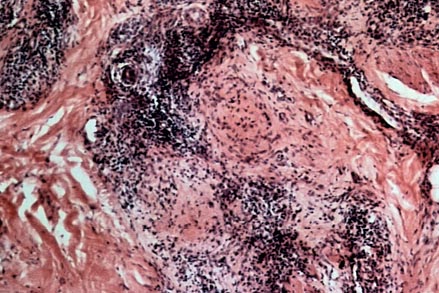
A punch biopsy of an involved area revealed a normal epidermis with epitheliod cell granulomas present in the dermis. Multinucleated giant cells were present in the reticular dermis and subcutaneous tissue. Polarization in search of foreign bodies was negative. PAS and Zeil-Nielson stains were negative.
A KOH preparation was negative. No growth was obtained on fungal and bacterial cultures.
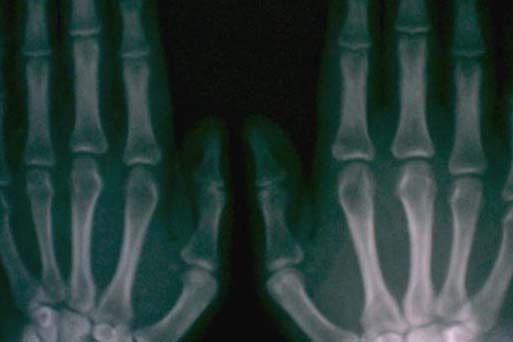
Chest and bone x-rays were normal. Hemoglobin and white blood cell counts were within normal range. Miscellaneous blood tests, including glucose, calcium, and creatinine were also normal.
 |  |
| Figure 3 | Figure 4 |
|---|---|
| Figures 3 and 4. Normal chest and bone x-rays. | |
Based on the above findings, a diagnosis was made of cicatricial alopecia due to sarcoidosis.
We opted to treat our patient with systemic steroids, because the scarring process was disfiguring his scalp and topical steroid therapy had been ineffective. We started with 40 mg daily for 4 weeks. The hair loss stopped but there was no regrowth. With a reduced dosage of prednisone, additional hair loss occurred. The dosage of prednisone was taken back to 40 mg / day, successfully halting the progression of his scarring alopecia.
Discussion
Sarcoidosis is a multisystem disease of unknown cause that may involve virtually any organ system . Because of its variable presentation, it may be difficult to diagnose. Diagnosis is made by the histopathological demonstration of granulomatous inflammation in the involved organs.[1] Cutaneous involvement may occur in as many as 25% of systemic sarcoidosis patients, and may also occur in the absence of systemic disease.[2] The diagnosis of cutaneous sarcoidosis is made on histological grounds. Although the diagnosis is often straightforward, the clinical and histological presentation of cutaneous sarcoidosis may sometimes be atypical.
The skin findings of sarcoidosis are categorized as non-specific or specific. Non-specific manifestations include reactive phenomena such as erythema nodosum. The specific cutaneous lesions of sarcoidosis are usually red or purple but can also be yellowish or reddish brown. They characteristically have a waxy, translucent appearance. Papules and nodules are common. Papules are found mostly around the eyes and in the nasolabial folds. Sometimes the papules may coalesce to form a ring that resembles granuloma annulare. Annular lesions can also result from plaques that are undergoing central atrophy. Cutaneous sarcoid nodules and plaques may mimic cutaneous T-cell lymphoma. Deep subcutaneous nodules and infiltration occur less commonly. Plaques with telangiectatic vessels on their surface have been described as angiolupoid sarcoidosis, while extensive plaques on earlobes, nose, fingers, and toes are known as lupus pernio.[3]
Involvement of the scalp is a rare manifestation of cutanous sarcoidosis. It may start as an atrophic, red, scaling area of alopecia, which must be distinguished histologically from chronic discoid lupus erythematosus of the scalp , lichen planopilaris, and scleroderma.[2] Local destruction and scarring of the follicles in sarcoidosis may lead to permanent alopecia, which is indistinguishable from Brocq pseudopalade.
Treatment options for sarcoidosis include antimalarials, immunosuppressive drugs, intralesional steroids, systemic steroids, and other drugs such as colchicine, allopurinol, and levamisol. At present, glucocorticoids are the most effective agents for influencing the course of cutaneous sarcoidosis. Oral prednisone in doses of 20 to 40 mg daily is the treatment of choice. Attempts to taper the dose usually begin after 4-6 weeks.[4]
A review of the English-language literature up to revealed only 28 reported cases. [1] Our case demonstrates, however, the severely disfiguring effects that can occur in these uncommon cases of scalp sarcoidosis.
References
1. Katta R, Nelson B, Chen D, Roenigk H. Sarcoidosis of the scalp: a case series and review of the literature. J Am Acad Dermatol. 2000 Apr;42(4):690-2. PubMed2. Rapp SE. An unusual cause of hair loss. Arch Dermatol. 2002 Feb;138(2):259-64. full text
3. Textbook of dermatology ROOK/ WILKINSON/EBLING C.D-ROM SIXTH EDITION
4. Dermatology in General Medicine, 5th Edition, cd-rom
© 2003 Dermatology Online Journal

