Abdominal wall ischemic fasciitis associated with a torso brace in a young girl
Published Web Location
https://doi.org/10.5070/D37s89x4d9Main Content
Abdominal wall ischemic fasciitis associated with a torso brace in a young girl
Sody A Naimer MD
Dermatology Online Journal 18 (11): 9
Department of Family Medicine, Siaal Research Center for Family Medicine and Primary Care, Faculty of Health Sciences, Ben-Gurion
University of the Negev, Beer-Sheva, Israel and Elon Moreh Clinic, Clalit Health Services, Shomron District, IsraelAbstract
We describe a rare case of ischemic fasciitis of the abdominal wall in a child with scoliosis. The fasciitis was apparently caused by the constant pressure exerted by her torso brace. Clinicians should be alert to the possibility of mechanical factors in the etiology of ischemic fasciitis.
Introduction
The manifestation of a hard mass in the soft tissue of cutaneous surfaces arouses concern in both patient and physician. The immediate challenge is to determine if it represents a life-endangering or benign condition. This is followed by collection of all possible information to assist in formulating the diagnosis. Both physical and external causes that may play a pathophysiologic role are evaluated.
Orthopedic conditions may be associated with cutaneous manifestations. We describe a unique case in which treatment of a congenital skeletal deformity resulted in a rare dermatological condition.
Case description
A 10-year-old girl presented to the local family health center with complaints of a “strange feeling” and tenderness of the skin in the area of the right lower abdomen, which had begun several days previously. The mother had noticed no other similar findings anywhere over the child’s body surface and was unaware of any such “sensations” in the past. The child had always been healthy and had never had any skin condition. She had not been wounded or subjected to trauma. The only remarkable finding on past medical history was significant idiopathic congenital scoliosis that was being treated by a torso brace, which the child had worn during all waking hours for the last two years (Figure 1).
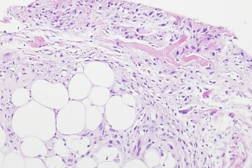
On physical examination, the cutaneous surface at the lower abdomen appeared normal. A small hard mass was palpated 1-2 cm medial to the right iliac crest, without dimpling the overlying skin. The mass was elongated (25-30 mm) and lay parallel to the inguinal ligament; it was mobile over the rectus abdominus muscle. Same-day tissue biopsy study yielded histopathologic findings of a fibrinous material (Figure 2). The pink area demonstrated by the arrow head features eosinophilic infiltration surrounded by reactive atypical fibroblasts, also infiltrating the underlying fat tissue (Figure 2, bottom). This pattern was consistent with a diagnosis of ischemic fasciitis. The excisional biopsy obliterated the lesion completely and therefore we cannot comment on the natural course of this phenomenon.
Discussion
Ischemic fasciitis is a rare pseudosarcomatous proliferation of atypical fibroblasts, located over bony protuberances. Unlike conventional fasciitis, the lesions are relatively large and believed to be associated with intermittent pressure on the soft-tissue structures, much like the ischemic basis of decubitus ulcer. Ischemic fasciitis was originally described as an ill-defined mass presenting in elderly bedridden or convalescent patients [1]. Ilaslan et al. [2] reported 3 severely debilitated patients with ischemic fasciitis over the greater trochanter region. More recently, however, in a larger series, Liegl and Fletcher [3] found that only 15 percent of patients were bedridden. All of the above authors stressed that the condition should be recognized as a reactive process distinct from soft tissue sarcoma. Others reported similar findings, which they termed atypical decubital fibroplasia, in the area of contact of a crutch in the forearm of a young man [4] and in an adolescent girl [5]. Our literature search did not yield any other reported cases in children.
In our patient, the involvement of pathologic tissue factors was unlikely given her young age and negative previous history of any dermatologic disorder. At the same time, the patient had been wearing a torso brace for 2 years for the treatment of scoliosis. On the basis of the close physical proximity of the rigid fixating bars of the orthopedic brace to the iliac crest, we assumed that the lesion was induced by friction or pressure on the deep subcutaneous tissues situated precisely under the brace tip.
This case raises questions regarding the unilateral presentation and the likelihood of such a tissue response. Were any subject-specific factors involved or was there an unknown factor that contributed to the localized sequence of events leading to tissue inflammation? This report should alert clinicians to the possibility of a mechanical factor in ischemic fasciitis.
Conclusions
Findings of a solitary nodule in pediatric practice should raise the possibility of friction between the body surface and a rigid external force. Padding may help to alleviate the heavier pressure exerted at the edges of fixating devices.
References
1. Perosio PM, Weiss SW, Ischemic fasciitis: a juxta-skeletal fibroblastic proliferation with a predilection for elderly patients, Mod Pathol. 6(1):69-72,1993. [PubMed]2. Ilaslan H, Joyce M, Bauer T, Sundaram M, Decubital ischemic fasciitis: Clinical, pathologic, and MRI features of pseudosarcoma, Am J Roentgenol. 187:1338-1341,2006. [PubMed]
3. Liegl B, Fletcher CD, Ischemic fasciitis: analysis of 44 cases indicating an inconsistent association with immobility or debilitation, Am J Surg Pathol. 32(10):1546-1552,2008. [PubMed]
4. Yamamoto M, Ishida T, Machinami R, Atypical decubital fibroplasia in a young patient with melorheostosis, Pathol Int. 48(2):160-163,1998. [PubMed]
5. Baranzelli MC, Lecomte-Houcke M, De Saint Maur P, Herbaux B, Pichon F, Deligny N, Demaille MC, Atypical decubitus fibroplasia: a recent entity. Apropos of a case of an adolescent girl, Bull Cancer. 83(1):81-84,1996. [PubMed]
© 2012 Dermatology Online Journal