Extramammary Paget disease of the penis as a manifestation of recurrent transitional cell carcinoma
Published Web Location
https://doi.org/10.5070/D37n68m3p4Main Content
Extramammary Paget disease of the penis as a manifestation of recurrent transitional cell carcinoma
Kathryn Somers1 MD, Luciano Iorizzo2 MD, Glynis Scott1,3 MD, Mary Gail Mercurio1 MD
Dermatology Online Journal 18 (8): 3
1. Department of Dermatology, University of Rochester Medical Center, Rochester, New York2. Department of Dermatology, Vanderbilt University Medical Center, Nashville, Tennessee
3. Department of Pathology, University of Rochester Medical Center, Rochester, New York
Abstract
Extramammary Paget disease (EMPD) mainly affects elderly women in areas with apocrine glands. Only 10 cases have been reported to involve the penis in patients with underlying transitional cell carcinoma of the bladder. Herein we report a patient with EMPD of the penis after radical cystectomy.
Extramammary Paget disease (EMPD) is an uncommon neoplastic skin condition affecting mainly elderly women in areas of the body with a large concentration of apocrine glands, such as the vulva [1]. EMPD affecting the penis and scrotum is a rare entity with about 150 cases previously reported [2]. There have been only ten reported cases of EMPD of the penis associated with underlying transitional cell carcinoma (TCC) [3]. We report a case of EMPD manifesting as a recurrence of TCC of the bladder status post radical cystectomy.
An 82-year-old man presented with a bleeding plaque around his urethral meatus, three years status post radical cystectomy with ileal conduit for Stage T3bN1MX transitional cell carcinoma. Examination of the penis revealed a well-demarcated red plaque on the glans with maceration and white discharge (Figure 1).
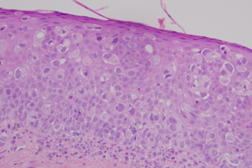
Histopathology was significant for large atypical cells throughout all levels of epidermis (Figure 2). The cells were strongly positive for cytokeratin 7 (CK7), cytokeratin 20 (CK20), epithelial membrane antigen, and pancytokeratin. Staining was negative for Melen-A and carcinoembryonic antigen. Stains for mucin were negative. These findings were diagnostic of EMPD; the dual staining of the tumor cells for CK7 and CK20 were consistent with spread from the underlying TCC rather than a primary EMPD [4]. After an unsuccessful trial of imiquimod, the plaque progressed to ulceration. Given that the patient no longer voided through his penis, was not sexually active, was in pain, and was at risk for infection, the decision was made to proceed with a partial penectomy, nearly five years after his initial diagnosis of TCC. The patient died two years after his partial penectomy at age 89, from complications of renal failure.
EMPD has been classified as either primary or secondary. Primary EMPD is an intraepidermal or adnexal adenocarcinoma without underlying malignancy, whereas secondary EMPD is associated with an underlying visceral malignancy [5]. The differentiation between primary and secondary EMPD prompts a discussion of the pathophysiology of the disease, which is not well understood. One theory posits that primary EMPD originates from multipotent stem cells within the skin and secondary EMPD is a cutaneous extension from the underlying visceral malignancy [2]. Primary and secondary EMPD look similar microscopically, but can be differentiated by immunohistochemical staining: EMPD extending from a visceral malignancy generally stains positive for both CK 7 and CK 20, whereas primary EMPD stains positive for CK7 but negative for CK 20 [4, 5]. EMPD of the glans penis as recurrence of a TCC is a rare entity and there is generally a long lag time in diagnosis of EMPD related to vague symptomatology and appearance. A prompt biopsy is reasonable after a patient with such a lesion does not improve after a brief course of topical treatment [1, 6]. Although it likely did not affect his outcome, this patient was not biopsied until 19 months following the development of his penile plaque. In the case of an elderly patient presenting with an erythematous plaque in an apocrine-dense region, it is prudent to consider that this may represent an undiagnosed visceral malignancy or, as in our case, the recurrence of a previously diagnosed malignancy. Prompt dermatologic evaluation and biopsy may prove helpful in the patient’s care.
References
1. Shepherd V, Davidson E, Davies-Humphreys J. Extramammary Paget’s disease. Br J Ob Gyn. 2005 Mar;112(3):273-9. [PubMed]2. Yang WJ, Kim DS, Im YJ, Cho KS, Rha KH, Cho NH, et al. Extramammary Paget’s disease of penis and scrotum. Urology. 2005 May;65(5):972-5. [PubMed]
3. Salamanca J, Benito A, Garcia-Penalver C, Azorin D, Ballestin C, Rodriguez-Peralto J. Paget’s disease of the glans penis secondary to transitional cell carcinoma of the bladder: a report of two cases and review of the literature. J Cutaneous Path. 2004 Apr;31(4):341-5. [PubMed]
4. Ohnishi T, Watanabe S. The use of cytokeratins 7 and 20 in the diagnosis of primary and secondary extramammary Paget’s disease. Br J Dermatol. 2000 Feb;142(2):243-7. [PubMed]
5. Lloyd J, Flanagan AM. Mammary and extramammary Paget’s disease. J Clin Path. 2000 Oct;53(10):742-9. [PubMed]
6. Smith D, Handy F, Evans J, Falzon M, Chapple C. Paget’s disease of the glans penis: an unusual malignancy. Eur Urol. 1994;25(4):316-9. [PubMed]
© 2012 Dermatology Online Journal