Retiform purpura: A new stigmata of illicit drug use?
Published Web Location
https://doi.org/10.5070/D33q1500t8Main Content
Retiform purpura: A new stigmata of illicit drug use?
Lauren Geller MD1, Talley B Whang MD1, Stephen E Mercer MD PhD2, Robert Phelps MD2
Dermatology Online Journal 17 (2): 7
1. Department of Dermatology, Mount Sinai Medical Center, New York, New York. Lauren.Geller@mssm.edu2. Division of Dermatopathology, Mount Sinai Medical Center, New York, New York
Abstract
We report a 50-year-old woman who presented with a six-month history of recurrent retiform purpura of uncertain etiology. Laboratory findings included neutropenia, positive anticardiolipin IgM antibody, and a weakly positive p-ANCA. Histopathology revealed a leukocytoclastic vasculitis with intravascular thrombi. Urine toxicology screen was positive for cocaine. These findings are similar to recent reports of agranulocytosis and purpura induced by levamisole-tainted cocaine. A review of the clinical and histopathological findings associated with levamisole-induced purpura will be discussed.
Introduction
Levamisole, originally developed as an antihelminthic and used in the past as an immunomodulatory agent, is now present as an adulterant in 70 percent of the US cocaine supply. Levamisole is rarely used in humans today because of its severe adverse effects including agranulocytosis and thrombotic vasculopathy resulting in retiform purpura. The latter tends to preferentially involve the earlobes and has been associated with positive autoantibodies, most commonly p- or c-ANCA and anticardiolipin. Lesions resolve without squelae two to three weeks after cessation of levamisole exposure.
Case report
A 50-year-old woman with a history of arthritis and substance abuse presented with a six-month history of recurrent purpuric patches on her trunk and extremities. The patches would heal within two weeks without treatment leaving atrophic scars. On physical exam, the patient had red-purple stellate purpura with central necrosis on her bilateral arms, breasts, and upper back (Figure 1a). She was also noted to have blue discoloration of her ears (Figure 1b). She was afebrile and had no systemic symptoms.
Laboratory studies were notable for a low white blood cell count (2,700 cells/mL) and an absolute neutrophil count of 1,400. Serum chemistries and coagulation studies were within normal limits. Blood cultures were negative. A comprehensive work up was performed to exclude hematologic and rheumatologic disorders that revealed positive anticardiolipin IgM antibodies, low-normal protein S Ag, weakly positive p-ANCA (titer 1:40), and a markedly elevated CRP of 44.3.
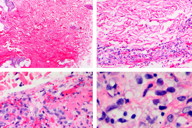
A skin biopsy showed severe vasculitis in all levels of the dermis with extensive intravascular fibrin thrombi. There was leukocytoclasis and erythrocyte extravasation (Figure 2). A prominent perivascular and periadnexal neutrophilic infiltrate was present, but special stains for organisms were negative.
There have been several recent reports of patients who used levamisole-tainted cocaine presenting with clinical findings similar to our patient. Given the negative workup for other causes of retiform purpura, we performed urine toxicology, which was positive for cocaine. Upon further questioning, our patient admitted to a relapse of cocaine use (after 18 years of sobriety) several weeks prior to the onset of the lesions.
Discussion
It has been reported that more than 70 percent of the US cocaine supply is being adulterated with levamisole [1]. Levamisole was originally prescribed as an antihelminthic and immunomodulatory agent but is no longer widely used in humans because of its serious side effects, including agranulocytosis and vasculitis. Although the reason why levamisole is added to cocaine remains unclear, it is speculated that levamisole may potentiate the addictive properties of cocaine by increasing dopamine levels in the brain [2].
The retiform purpura associated with levamisole adulterated cocaine use is characterized histopathologically by thrombotic vasculitis or leukocytoclastic vasculitis with or without vascular occlusion. The skin lesions may appear anywhere on the body, but tend to preferentially involve the external ear. Lesions have a distinctive morphology; they tend to be stellate with a bright erythematous border and necrotic appearing center. Spontaneous resolution will occur upon cessation of the offending agent. An association with positive anticardiolipin antibody and c- or p-ANCA, as seen in our patient, has been reported [3].
There may be a concomitant life-threatening agranulocytosis, which is more commonly reported in patients carrying the HLA-B27 genotype [4]. It is possible that the retiform purpura is also associated with HLA-subtypes, which could explain why levamisole induces vasculitis in some and not others.
Because of the short half-life of levamisole and the limited availability of the lab tests needed to detect this contaminant, we were unable to confirm that the cocaine in her possession was adulterated with levamisole. However, the temporal relationship of her cocaine use with the onset of symptoms, the purpuric lesions involving the ears, and the characteristic lab findings were strongly suggestive of levamisole toxicity.
Levamisole-induced purpura is being seen at a markedly increased rate across the United States. Given that more than 2 million Americans use cocaine monthly, the high frequency with which the cocaine in the United States is adulterated with levamisole poses a serious public health risk. There should be an increased awareness of the cutaneous findings associated with levamisole-tainted cocaine. If a patient presents with localized purpuric lesions, particularly involving the earlobes, a careful drug history should be taken and toxicology studies should be performed.
References
1. Centers for Disease Control and Prevention (CDC). Agranulocytosis associated with cocaine use – four states, March 2008-November 2009. MMWR Morb Mortal Wkly Rep 2009:58;1381-1385. [PubMed]2. Buchanan JA, Oyer RJ, Patel NR, Jacquet GA, et al. A confirmed case of agranulocytosis after use of cocaine contaminated with levamisole. J Med Toxicol 2010:6;160-164. [PubMed]
3. Waller JM, Feramisco JD, Alberta-Wszolek L, McCalmont TH, et al. Cocaine-associated retiform purpura and neutropenia: Is levamisole the culprit? J Am Acad Dermatol 2010;63:530-535. [PubMed]
4. Czuchlewski DR, Brackney M, Ewers C, Manna J, et al. Clinicopathologic features of agranulocytosis in the setting of levamisole-tainted cocaine. Am J Clin Pathol 2010;133:466-472. [PubMed]
© 2011 Dermatology Online Journal