Secondary follicular mucinosis associated with systemic lupus erythematosus
Published Web Location
https://doi.org/10.5070/D39sj6f46jMain Content
Secondary follicular mucinosis associated with systemic lupus erythematosus
Kathryn O’Reilly MD PhD, Jeremy Brauer MD, Aaron Lloyd MD, Rishi Patel MD, Ruth Walters MD, Andrew G Franks Jr MD
Dermatology Online Journal 16 (11): 7
Department of Dermatology, New York University, New York, New YorkAbstract
A 61-year-old woman presented with a five-month history of an intermittent eruption of papules and nodules on her face and neck. Past medical history included systemic lupus erythematosus. Histopathologic examination was consistent with secondary follicular mucinosis in association with systemic lupus erythematosus. This rare entity has been described in one prior report as a precursor to the clinical onset of systemic lupus erythematosus. Follicular mucinosis occurs as either a primary idiopathic form or a secondary form associated with either benign inflammatory processes or malignant conditions, such as cutaneous T-cell lymphoma. Numerous treatments for primary follicular mucinosis have been described, which include isotretinoin and glucocorticoids, whereas treatment of the underlying disease is necessary in the secondary form. The association with lymphoma mandates long-term clinical monitoring of patients with particularly recalcitrant, widespread, or chronic follicular mucinosis.
History
 |  |
| Figure 1 | Figure 2 |
|---|
 |
| Figure 3 |
|---|
A 61-year-old woman presented to the Charles C. Harris Skin and Cancer Pavilion for evaluation of a five-month history of an intermittent eruption on the face and neck. She had experienced weekly outbreaks over the past five months that consisted of tender, pruritic lesions on the face and neck. The patient had been evaluated by a dermatologist who started her on a six-week regimen of doxycycline, hydrocortisone cream, and a topical antibiotic. The eruption did not improve, so the patient had discontinued these treatments two months prior to her presentation. She had ceased using face wash, moisturizer, and sunscreen for fear that “they will break me out.”
Past medical history included systemic lupus erythematosus without cutaneous involvement that was diagnosed in 1984 and managed at an outside hospital. The last flare of lupus erythematosus was one year prior to presentation and systemic manifestations have included fever, weakness, arthralgias, headaches, and arthritis. Past medical history also included hypertension and coronary artery disease. Medications included imdur, metoprolol, and a multivitamin. She denied drug allergies, alcohol consumption, or tobacco use. Pertinent family history included lupus erythematosus in the patient’s mother who passed away at 34 years of age from complications. Review of systems was negative.
Physical examination
Erythematous and hyperpigmented papules and nodules, some with fine scale, were scattered on forehead, cheeks, nose, chin, and anterior aspect of the neck.
Laboratory data
A complete blood count with differential analysis, metabolic panel, liver function tests, and lipid panel were normal. An anti-nuclear antibody test showed a 1:160 titer with a speckled pattern.
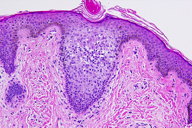
Histopathology
There is a superficial and deep, perivascular and perifollicular, infiltrate of lymphocytes and numerous eosinophils. Lymphocytes extend into the follicular epithelium where findings include spongiosis and slightly increased deposits of connective-tissue mucin, as highlighted by a colloidal-iron stain. Lymphocytes contain small nuclei with regular contours.
Comment
Follicular mucinosis was first described by Pinkus in 1957. At the time, he reported six cases of alopecia mucinosa, which is a focal alopecia with mucin deposition in hair follicles [1]. In 1959, the condition was renamed follicular mucinosis inasmuch as alopecia often was absent [2]. Follicular mucinosis is an uncommon, chronic, inflammatory condition, which often occurs in children and adults in the third and fourth decades of life [3]. Although follicular mucinosis commonly presents as shiny, pink or skin-colored, follicular papules or plaques with scale, several distinct clinical presentations have been described, which include nodules, annular plaques, folliculitis, and acneiform lesions [4, 5].
Follicular mucinosis may occur as a primary entity, which is a benign idiopathic form that is not associated with other cutaneous or extracutaneous diseases. The primary form usually is limited to the face and scalp with associated alopecia. Alternatively, secondary follicular mucinosis is associated with benign inflammatory conditions, such as atopic dermatitis, or malignant conditions, such as cutaneous T-cell lymphoma [6]. Secondary follicular mucinosis is characterized by larger, more numerous plaques, more widespread involvement, a more chronic clinical course, and/or an older age group than is the primary form [1, 7]. Follicular mucinosis associated with lupus erythematosus is a rare entity. A Pubmed literature search produced only one case report of a patient with follicular mucinosis that was associated with systemic lupus erythematosus [8]. In this case, follicular mucinosis was described as a precursor to clinical and serologic evidence of systemic lupus erythematosus, which was similar to a report of papulonodular mucinosis and systemic lupus erythematosus [8, 9].
Histopathologic features of follicular mucinosis include mucin deposition in the epithelium of the follicular outer root sheath and sebaceous glands [10]. The mechanism for selective deposition of mucin in the epithelium of the hair follicle remains unknown. Although primary follicular mucinosis may resolve spontaneously, many successful treatments have been reported, which include indomethacin; topical, intralesional, and systemic glucocorticoids; dapsone; topical tretinoin; oral isotretinoin; minocycline; tetracycline; and psoralen with ultraviolet A photochemotherapy [11, 12]. Treatment of secondary follicular mucinosis requires treatment of the underlying condition. As cases of follicular mucinosis progressing to cutaneous T-cell lymphoma have been reported, patients with persistent or widespread disease should be monitored longitudinally [1].
References
1. Pinkus H. Alopecia mucinosa: inflammatory plaques with alopecia characterized by root-sheath mucinosis. Arch Dermatol 1957; 76:419 [PubMed]2. Jablonska S, et al. Mucinosis follicularis. Hautarzt 1959; 10:27 [PubMed]
3. Cerroni L, et al. Follicular mucinosis: a critical reappraisal of clinicopathologic features and association with mycosis fungoides and Sézary syndrome. Arch Dermatol 2002;138: 182 [PubMed]
4. Passaro EM, et al. Acneiform follicular mucinosis. Clin Exp Dermatol 2004; 29:396 [PubMed]
5. Muscardin LM, et al. Acneiform follicular mucinosis of the head and neck region. Eur J Dermatol 2003; 13:199 [PubMed]
6. Parker SR , Murad E. Follicular mucinosis: clinical, histologic, and molecular remission with minocycline. J Am Acad Dermatol 2009 Jul 24 [Epub ahead of print]. [PubMed]
7. Rongioletti F, et al. Follicular mucinosis: a clinicopathologic, histochemical, immunohistochemical and molecular study comparing the primary benign form and the mycosis fungoides-associated follicular mucinosis. J Cutan Pathol. 2009 Jul 14. [Epub ahead of print]. [PubMed]
8. Dawn G, et al. Follicular mucinosis and systemic lupus erythematosus. Dermatology 1997;195:183 [PubMed]
9. Rongioletti F, Rebora A. Papular and nodular mucinosis associated with systemic lupus erythematosus. Br J Dermatol 1986; 115:631 [PubMed]
10. Anderson BE, et al. Alopecia mucinosa: report of a case and review. J Cutan Med Surg 2003;7:124 [PubMed]
11. Arca E, et al. Follicular mucinosis responding to isotretinoin treatment. J Dermatolog Treat 2004; 15:391 [PubMed]
12. Guerriero C, et al. Follicular mucinosis successfully treated with isotretinoin. Eur J Dermatol 1999; 9:22 [PubMed]
© 2010 Dermatology Online Journal

