Atypical mycobacteria infection in an immunocompromised patient
Published Web Location
https://doi.org/10.5070/D33s91k3t0Main Content
Atypical mycobacteria infection in an immunocompromised patient
Emily Berger MD, Priya Batra MD, Jonathan Ralston MD, Miguel R Sanchez MD, Andrew G Franks Jr MD
Dermatology Online Journal 16 (11): 21
Department of Dermatology, New York University, New York, New YorkAbstract
A 61-year-old woman with systemic lupus erythematosus and Sjögren syndrome presented with a two-month history of symptomatic nodules on the buttocks and thighs that progressed to involve the dorsal aspects of the hands. On examination, infiltrative papules, nodules, and plaques were present in these regions. Biopsy specimens demonstrated granulomatous inflammation and acid-fast bacilli with the use of a Fite stain, although a culture and polymerase chain reaction analysis were negative. The patient continues to improve on long-term clarithromycin therapy. Atypical mycobacterial infections are becoming more common, especially in immunocompromised patients. Antimicrobial therapy, either with a single agent or multiple agents, often is prolonged. A high index of suspicion is warranted in immunocompromised patients, which includes those with connective-tissue diseases that are active or that require immunosuppression. In these patients, the differential diagnosis includes infectious as well as inflammatory, reactive, or neoplastic processes.
History
 |  |
| Figure 1 | Figure 2 |
|---|
A 61-year-old woman with systemic lupus erythematosus and Sjögren syndrome presented to the Dermatology Consult Service at Bellevue Hospital Center in August, 2009, with a two-month history of enlarging, painful and pruritic lesions of the hips and thighs. In September, 2009, she presented to the Dermatology Clinic for further evaluation with a three-week history of swollen, red papules and nodules overlying the joints of her hands. With the exception of intermittent shortness of breath, she felt well without fevers, chills, or weight loss. Past medical history included interstitial lung disease and hypertension. Medications included low-dose prednisone, hydroxychloroquine, and azathioprine. There was no recent history of trauma, fish-tank exposure, or travel outside the New York area. After a series of skin biopsies were taken, clarithromycin 500 mg was initiated twice daily with slow improvement of lesions on the buttocks, thighs, and hands.
Physical examination
On the lateral aspects of the hips and buttocks, there were erythematous-to-violaceous, non-scaling papules and plaques with warmth to palpation. On the left hip were compressible nodules without drainage. On the hands, there were erythematous papulonodules with scale overlying some proximal interphalangeal and metacarpalphalangeal joints.
Laboratory data
A complete blood count was normal. Erythrocyte sedimentation rate was elevated at 45 mm/hr and C-reactive protein was elevated at 11.54 mg/dL. C3 and C4 were normal; double-stranded DNA antibody was <1.
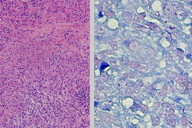
Histopathology
There is granulomatous inflammation with areas of necrosis and some Langerhans-type giant cells. A Fite stain shows scattered acid-fast bacilli.
Comment
Atypical mycobacteria infections are those that are not caused by Mycobacterium tuberculosis or M. leprae. Prevalent in the environment, atypical mycobacteria are an increasing cause of cutaneous infections, especially in immunocompromised patients. Atypical mycobacteria are classified based on fast or slow growth and their ability to produce pigment. Slow-growing atypical mycobacteria include M. marinum, M. kansasii, and M. avium-intracellulare. Fast-growing atypical mycobacteria include M. fortuitum, M. chelonei, and M. abscessus. The clinical presentation of skin disease is dependent on the causative organism and includes but is not limited to, papules, plaques, nodules, abscesses, and ulcers. Histopathologic patterns may include nonspecific dermal or subcutaneous histiocytic inflammation, abscesses, tuberculoid or sarcoidal granulomas, and rheumatoid-like nodules [1]. Tissue cultures are needed to establish the diagnosis [2]. Polymerase chain reaction analysis of tissue samples is a diagnostic modality that may increase sensitivity and specificity of diagnosis [3]. Diagnosis often is delayed [4]. Therapy will vary depending on the causative agent [5]. Antimicrobial treatment may be initiated empirically to avoid progression; however, ideal therapy is tailored to the results of culture data. In one retrospective study of 25 cases of non-tuberculous mycobacterial skin infection, in which M. marinum was isolated in most cases, clarithromycin was the drug of choice based on susceptibility and clinical response [1]. Monotherapy with clarithromycin also has had success in a patient with systemic lupus erythematosus and cutaneous M. szulgai infection [6]. Other authors advocate multi-drug regimens to avoid antimicrobial resistance [7]. Regardless of the choice of antibiotics, therapy is of several months to greater than one-year duration. Surgical intervention also may be employed [5].
There are reports of disseminated disease and deeper soft tissue and musculoskeletal infections in immunocompromised patients, which includes those with systemic lupus erythematosus (SLE) [8]. Dissemination, however, is rare. A retrospective study of 11 cases of culture-positive, non-tuberculous mycobacterial infections in patients with SLE found that 8 of 11 patients had isolated involvement of skin or soft tissues, which included nodules, abscesses, ulcers, or synovitis. Only one patient had disseminated involvement [4].
Immunocompromise in patients with connective-tissue diseases may relate either to the active disease or immunosuppressive agents used to treat the disease. A high index of suspicion for atypical mycobacteria infection is important in the evaluation of new or atypical skin lesions. As in our patient, the differential diagnosis includes connective-tissue diseases [2] rheumatoid nodules, palisaded and neutrophilic granulomatous dermatitis, erythema elevatum diutinum, Hansen disease, deep fungal infection, and malignant conditions.
References
1. Dodiuk-Gad R, et al. Nontuberculous mycobacterial infections of the skin: a retrospective study of 25 cases. J Am Acad Dermatol 2007; 57: 413 [PubMed]2. Czelusta A, Yen Moore A. Cutaneous Mycobacterium kansasii infection in a patient with systemic lupus erythematosus: case report and review. J Am Acad Dermatol 1999; 40: 359 [PubMed]
3. Martinez Zugaib Abdalla C, et al. Polymerase chain reaction compared to other laboratory findings and to clinical evaluation in the diagnosis of cutaneous tuberculosis and atypical mycobacteria skin infection. Int J Dermatol 2009; 48:27 [PubMed]
4. Mok MY, et al. Non-tuberculous mycobacterial infection in patients with systemic lupus erythematosus. Rheumatology 2007; 46: 280 [PubMed]
5. Bolognia J, et al. eds. Mycobacterial Infections.Dermatology, 2nd edition. London: Mosby, 2008: 1119
6. Shimizu T, et al. Successful treatment using clarithromycin for a cutaneous lesion caused by Mycobacterium szulgai. Br J Dermatol 2000; 142: 838 [PubMed]
7. Bhambri S, et al. Atypical Mycobacterial cutaneous infections. Dermatol Clin 2009; 27: 63 [PubMed]
8. Enzenauer RJ, et al. Disseminated cutaneous and synovial Mycobacterium marinum infection in a patient with systemic lupus erythematosus. South Med 1990; 83: 471 [PubMed]
© 2010 Dermatology Online Journal

