Porokeratosis palmaris et plantaris disseminata or a disseminated late-onset variant of porokeratotic eccrine ostial and dermal ductal nevus (PEODDN) with follicular involvement
Published Web Location
https://doi.org/10.5070/D33b86872rMain Content
Porokeratosis palmaris et plantaris disseminata or a disseminated late-onset variant of porokeratotic eccrine ostial and dermal
ductal nevus (PEODDN) with follicular involvement
Rachael Hartman MD, Carina Rizzo MD, Rishi Patel MD, Hideko Kamino MD, Jerome L Shupack MD
Dermatology Online Journal 15 (8): 8
Department of Dermatology, New York UniversityAbstract
A 48-year-old woman presented with a four-year history of pruritic, hyperkeratotic, spiny papules that began on her chest and spread to her extremities, groin, palms, face, and scalp where it caused non-scarring alopecia. Histopathologic features included cornoid lamella, which is the hallmark of porokeratosis. However, the patient's constellation of findings does not meet diagnostic criteria for any of the five clinical variants of porokeratosis. Her presentation is most compatible with either porokeratosis palmaris et plantaris disseminata (PPPD), which is a rare variant of punctate porokeratosis that can involve any area of the body or late-onset porokeratotic eccrine ostial and dermal ductal nevus (PEODDN), which is a rare, benign hamartoma of the eccrine sweat glands with porokeratotic histopathologic features that has been reported to occasionally have systemic involvement. Treatment of either condition is difficult although there have been reported successes with cryotherapy, surgical excision, and CO2 laser. Since porokeratosis is a disorder of keratinization and our patient has prominent follicular involvement, isotretinoin may be another reasonable therapeutic option.
History
 |  |
| Figure 1 | Figure 2 |
|---|---|
 |
| Figure 3 |
|---|
A 48-year-old woman presented to an outside dermatologist in 2004, with a pruritic eruption on her chest that began around the same time that a diagnosis of hypothyroidism was made. Her skin lesions gradually spread to her extremities, buttocks, and groin. She was evaluated by numerous dermatologists and had multiple shave and punch biopsies; most of the biopsy specimens were suggestive of porokeratosis although one was interpreted as verruca vulgaris and another as acantholytic dyskeratosis. The patient was initially treated with topical glucocorticoids, antihistamines, and oral antibiotics with no improvement. From October, 2007, through January, 2008, she was treated with acitretin and PUVA photochemotherapy; the treatment was discontinued because the patient reported a worsening of her symptoms and a more rapid spread of the lesions to her scalp, buttocks, and groin. In late 2007, she developed alopecia on the crown of her head. In June, 2008, the lesions spread to her face and to the palms.
The patient presented to Dr. Jerome Shupack's office in September, 2008. She complained of pruritus and serous drainage from her genital lesions. She denied recent travel, fevers, chills, and headaches. Doxycycline 150 mg daily, Carmol 40, and tramadol were initiated. She reported some improvement with doxycycline, particularly of her facial lesions.
Medical history includes hypothyroidism. Surgical history includes thyroidectomy due to thyroid nodules and five surgical procedures of the feet between 1989 and 2005. Current medications include Armour thyroid tablets (a natural thyroid replacement therapy containing both T3 and T4), doxycycline, Carmol 40, and tramadol. She has no family history of skin disease.
Physical Examination
On the arms and legs were multiple, small, erythematous, hyperkeratotic papules in a follicular distribution. Many of the papules had thin spinous processes and were rough to the touch. On the trunk and abdomen were similar lesions although they were sparser and more linearly arranged. On the palmar surface of both hands were approximately 15 larger, raised papules with central keratinous plugs. The soles were clear. On the chin and cheeks were larger papulonodules on an erythematous base. There was non-scarring alopecia on the crown of the scalp, with yellow, filiform papules and yellow crust at the base. Behind the ears were scattered, filiform papules with fine white spicules that were often adherent to the surrounding hair. The vulva, perineum, gluteal region, and inner thighs were covered with a mixture of small spiny papules, larger umbilicated papules, and inflamed nodules, some of which were connected by tracts, and others of which were eroded with serous drainage.
Laboratory data
A complete blood cell count with differential analysis and a comprehensive metabolic panel were normal. Epstein Barr viral capsid antigen IgG antibody and Epstein Barr nuclear antigen IgG antibody were positive at 2315 AU/mL and 270 AU/mL, respectively. Heavy metal blood panel was negative for arsenic, mercury, and lead. Thyroid stimulating hormone, T3, and T4 levels have been normal since the patient has been on replacement therapy. Cultures for Neisseria gonorrhoeae and Chlamydia species were negative. Anti-SS-A antibody was normal.
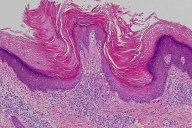
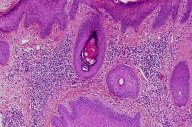
Histopathology
There is a dense, perifollicular infiltrate of lymphocytes and histiocytes. Several follicles have a dialated infundibulum with cornoid lamellae, underlying hypogranulosis, and dyskeratotic cells. In a biopsy specimen from the scalp, there is one cornoid lamella that involves the inferior segment of the hair follicle.
Comment
Porokeratosis is disorder of epidermal keratinization, which is characterized by hyperkeratotic papules or plaques that are surrounded by a thread-like elevated border [1, 2, 3]. The histopathologic hallmark of porokeratosis is the cornoid lamella, which is a thin column of parakeratosis that overlies a thin or absent granular layer and that corresponds to the raised, hyperkeratotic border observed clinically. The underlying dermis often shows a lymphohistiocytic infiltrate [1].
At least five distinct clinical variants of porokeratosis have been recognized: porokeratosis of Mibelli, disseminated superficial porokeratosis, disseminated superficial actinic porokeratosis (DSAP), linear porokeratosis, and punctate porokeratosis of the palms and soles [3]. There are reports of more than one type of porokeratosis developing in the same patient. Disseminated porokeratosis has been reported in patients with immunosuppression due to systemic diseases, organ transplantation, and medications [3].
The differential diagnosis of porokeratosis also includes porokeratotic eccrine ostial and dermal ductal nevus (PEODDN), which is a rare, benign hamartoma of the eccrine sweat glands with porokeratotic histopathologic features [4]. Porokeratotic eccrine ostial and dermal ductal nevus typically presents with linearly-distributed, keratotic papules or plaques with central plugged pits, which occur commonly on the distal aspects of extremities [5]. However, several cases of systematized, widespread distribution have been reported [4, 6, 7]. Our patient had alopecia, and a case of PEODDN with widespread bilateral involvement that included severe alopecia, onychodysplasia, and palmoplantar involvement has been reported [4].
Although PEODDN is typically congenital, there are several case reports of the onset of PEODDN in adults [8, 9, 10, 11]. The frequency of late-onset PEODDN may be as high as 26 percent [8]. The onset of our patient's symptoms also coincided with her diagnosis of thyroid disease. Interestingly, a 66-year-old man with late-onset PEODDN associated with hyperthyroidism has been reported although it is unclear whether the association was coincidental or causally related [10].
Whereas our patient had the characteristic cornoid lamella on histopathologic examination, her clinical presentation and histopathologic features were difficult to correlate with any of the standard variants of porokeratosis. Her case most closely resembles porokeratosis palmaris et plantaris disseminata (PPPD), which is a rare variant of punctuate porokeratosis that can involve any area of the body, or late-onset PEODDN. However, neither diagnosis is characteristic of this patient. Porokeratosis palmaris et plantaris disseminata usually begins on the palms and soles, whereas our patient's palms were not involved until later in her course and her soles were clear. As for PEODDN, the cornoid lamellae are usually located in the eccrine ostia, whereas the cornoid lamellae in our patient were follicular.
Porokeratosis has been treated with cryotherapy, topical 5-fluorouracil with and without topical retinoids, imiquimod, CO2 and other lasers, shave excision, curettage, linear excision, and dermabrasion, with variable success [12, 13, 14, 15]. Acitretin has been reported to treat widespread and refractory lesions although the disease recurs following its discontinuation [16]. Because porokeratosis is a disorder of keratinization and our patient has prominent follicular involvement, isotretinoin may be another therapeutic option. A case of PPPD was successfully treated with isotretinoin [17].
Treatment options for PEODDN include topical glucocorticoids under occlusion, calcipotriol ointment, cryotherapy, electocautery, and surgical excision, although PEODDN tends to be resistant to treatment [10]. A case of PEODDN with widespread involvement that was treated with ultrapulsed CO2 laser with good results has been reported [6].
References
1. Robinson JB, et al. Vulvar porokeratosis: case report and review of the literature. Int J Gynecol Pathol 1999; 18: 169 [PubMed]2. de Almeida HL Jr, et al. Follicular involvement in porokeratosis. J Eur Acad Dermatol Venereol 2007; 21: 109 [PubMed]
3. Kanekura T, Yoshii N. Eruptive pruritic papular porokeratosis: a pruritic variant of porokeratosis. J Dermatol 2006; 33: 813 [PubMed]
4. Kroumpouzos G, et al. Systematized porokeratotic eccrine and hair follicle naevus: report of a case and review of the literature. Br J Dermatol 1999; 141: 1092 [PubMed]
5. Sassmannshausen J, et al. Porokeratotic eccrine ostial and dermal ductal nevus: a case report and review of the literature. J Am Acad Dermatol 2000; 43: 364 [PubMed]
6. Leung CS, et al. Porokeratotic eccrine ostial and dermal duct naevus with dermatomal trunk involvement: literature review and report on the efficacy of laser treatment. Br J Dermatol 1998; 138: 684 [PubMed]
7. Cobb MW, et al. Porokeratotic eccrine ostial and dermal ductal nevus: a case of systematized involvement. Cutis 1999; 46: 495 [PubMed]
8. Valks R, et al. Porokeratotic eccrine ostial and dermal ductal nevus of late onset: more frequent than previously suggested? Dermatology 1996; 193: 138 [PubMed]
9. Birol A, et al. A case report of porokeratotic eccrine ostial and dermal ductal naevus of late onset. J Eur Acad Dermatol Venereol 2004; 18: 619 [PubMed]
10. Rasi A, Tajziechi L. Late-onset porokeratotic eccrine ostial and dermal ductal nevus associated with sensory polyneuropathy and hyperthyroidism. Arch Iran Med 2008; 11: 218 [PubMed]
11. Stoof TJ, et al. Porokeratotic eccrine ostial and dermal ductal nevus: report of a case of adult onset. J Am Acad Dermatol 1989; 20: 924 [PubMed]
12. Shumack SP, Commens CA. Disseminated superficial actinic porokeratosis: a clinical study. J Am Acad Dermatol 1989; 20: 1015 [PubMed]
13. McDonald SG, Peterka ES. Porokeratosis (Mibelli): treatment with topical 5- fluorouracil. J Am Acad Dermatol 1983: 8: 107 [PubMed]
14. Rabbin PE, Baldwin HE. Treatment of porokeratosis of Mibelli with CO2 laser vaporization versus surgical excision with split-thickness skin graft: a comparison. J Dermatol Surg Oncol 1993; 19: 199 [PubMed]
15. Spencer JM, Katz BE. Successful treatment of porokeratosis of Mibelli with diamond fraise abrasion. Arch Dermatol 1992; 128: 1187 [PubMed]
16. Goldman GD, Milstone LM. Generalized linear porokeratosis treated with etretinate. Arch Dermatol 1995; 131: 496 [PubMed]
17. McCallister RE, et al. Porokeratosis plantaris, palmaris, et disseminata: report of a case and a treatment with isotretinoin. J Am Acad Dermatol 1985; 13: 598. [PubMed]
© 2009 Dermatology Online Journal

