Subcorneal pustular dermatosis in a patient with rheumatoid arthritis and diffuse scleroderma
Published Web Location
https://doi.org/10.5070/D38qx0t9w5Main Content
Subcorneal Pustular Dermatosis in a Patient with Rheumatoid Arthritis and Diffuse Scleroderma
Elise I Brantley MD1, Pranav Sheth MD2
Dermatology Online Journal 15 (3): 5
1. Dermatology Resident2. Assistant Professor of Dermatology
Department of Dermatology, University of Cincinnati, Ohio. pranav.sheth@uc.edu
Abstract
We report a case of subcorneal pustular dermatosis (SPD) in a patient with rheumatoid arthritis (RA) and diffuse scleroderma. Although SPD has been described in association with RA, it has not been reported in association with diffuse scleroderma to our knowledge. This observation supports the hypothesis linking immune dysfunction as a common pathogenesis of these three entities.
Introduction
Subcorneal pustular dermatosis (SPD) of Sneddon and Wilkinson was first described in 1956 [1]. It is a rare disorder characterized by recurrent "crops" of discrete sterile vesiculopustules. SPD has been reported alone and in association with multiple systemic autoimmune disorders, hypergammaglobulinemias, and neoplasms. We report a case of subcorneal pustular dermatosis associated with diffuse scleroderma and rheumatoid arthritis.
Case Report
A 37-year-old African-American female presented with a pruritic, occasionally painful, chronic blistering eruption of one-year duration involving the abdomen, back, and thighs. She had received several short courses of systemic steroid tapers followed by rapid recurrence, and subsequently longer term tapering prednisone. At the time of her initial visit, she was on prednisone 2.5 mg for 3 months with continued moderate activity. Her past medical history was significant for rheumatoid arthritis and diffuse scleroderma for 10 years. Her medications included atenolol, valsartan, hydroxychloroquine, furosemide, nifedipine, and naprosyn, all of which had been given for over one year.
On physical exam, involving the chest, back, abdomen, and thighs there were numerous, 2-6 mm superficial vesicles and pustules, some of which exhibited the meniscus sign (Figs. 1a & 1b). The lesions were on a background of hyperpigmented round macules. Her fingertips had a slight, firm taper and early sclerodactyly. She had marked joint deformities of the proximal interphalangeal joints and slight ulnar deviation at the metacarpophalangeal joints bilaterally. Her mucous membranes were clear.
 |  |
| Figure 2 | Figure 3 |
|---|---|
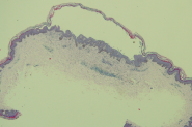
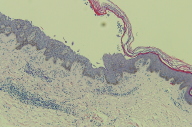
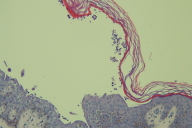
| Figures 2-4. A subcorneal pustule containing few neutrophils and acantholytic cells | |
 |
| Figure 4 |
|---|
The differential diagnosis included pustular psoriasis, dermatitis herpetiformis, pemphigus foliaceus, subcorneal-type IgA pemphigus, and subcorneal pustular dermatosis. Histopathology revealed a subcorneal vesicle with few neutrophils and epidermal acantholytic cells (Figs. 2-4). The superficial dermis revealed a moderate lymphocytic infiltrate with neutrophils and eosinophils. Direct immunofluorescence was negative on two occasions. Indirect immunofluorescence using salt split skin and monkey esophagus was negative. These findings were consistent with subcorneal pustular dermatosis of Sneddon and Wilkinson.
Given the patient's multiple other medical problems and medications, she was started on Dapsone 50 mg a day in addition to the prednisone 2.5 mg. She had rapid clearance of her skin within two weeks. After two months, a flare with new lesions prompted an increase of the Dapsone to 100 mg daily. This resulted in complete and sustained clearance at all subsequent visits during a follow up period of nine months.
Discussion
Subcorneal pustular dermatosis (SPD) of Sneddon and Wilkinson is a rare disorder presenting with recurrent sterile vesicopustules. It generally affects women in the third decade or older and runs a benign yet chronic course. Subcorneal pustular dermatosis typically responds rapidly to dapsone, though other treatment options have been reported including colchicine, PUVA, UVB, cyclosporine, and infliximab [2, 3, 4, 5].
Differentiating SPD from other causes of superficial vesiculopustular eruptions can be challenging. Clinically, the lack of systemic symptoms, the lack of confluence of the pustules, and the larger size of the pustules puts pustular psoriasis lower on the differential. Histopathology and immunofluorescence are needed to rule out the other entities. On histopathology, lesions demonstrating a sterile subcorneal pustule rule out dermatitis herpetiformis. The minimal findings of acantholysis do not lend themselves to the various forms of pemphigus, nor do the negative immunofluorescence studies.
Subcorneal pustular dermatosis has been reported alone and in association with many disorders including seropositive and seronegative rheumatoid arthritis (RA), Sjögren disease, Crohn disease, systemic lupus erythematosus, Grave disease, multiple sclerosis, pyoderma gangrenosum, synovitis-acne-palmoplantar-pustulosis-hyperosteosis-osteitis (SAPHO) syndrome, benign monoclonal IgA, IgG, and IgM gammopathy, acquired immune deficiency syndrome, multiple myeloma, apudoma, and pancreatic cancer [6-26]. The etiology of SPD is largely unknown, but given its association with several autoimmune disorders and hyperimmunoglobulinemia, some have proposed an underlying autoimmune etiology or systemic immunologic defect.
The association between RA and SPD has been noted for some time. There are many proposed theories linking the pathogenesis of the two entities. The activation and chemotaxis of neutrophils is intimately involved in the pathogenesis of both conditions, as is up regulation of many cytokines and chemokines, including interleukin (IL)-8 and tumor necrosis factor (TNF)-alpha [9, 14, 27, 28].
The pathogenesis of diffuse scleroderma involves immune dysregulation and a cascade of synergistic events including endothelial cell damage, activation of T cells, proinflammatory and profibrotic cytokine production, inflammation, and activation of fibroblasts [29]. Immune dysregulation plays a key role in many of the other diseases found to be associated with SPD, including multiple sclerosis, monoclonal IgA gammopathies, and SLE [15, 17, 20, 22, 30]. The coexistence of diffuse scleroderma and SPD in our patient supports the hypothesis that immune dysregulation may play a role in the pathogenesis of SPD.
Summary
Subcorneal pustular dermatosis is a chronic blistering disorder that affects young to middle-aged women. In our patient, SPD was associated with underlying RA and diffuse scleroderma. The rapid response to dapsone probably speaks to the presence of neutrophils seen histologically. Though the etiology is poorly understood, its association with immunologic disorders such as RA and scleroderma may offer insight into its pathogenesis.
References
1. Sneddon IB, Wilkinson DS. Subcorneal pustular dermatosis. Br J Dermatol 1956;68:385-394. [PubMed]2. Kouchemoune A, Blyumin ML. Sneddon-Wilkinson disease resistant to dapsone and colchicine successfully controlled with PUVA. Dermatol Online J. 2003 Dec;9(5):24. [PubMed]
3. Cameron H, Dawe RS. Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) treated with narrowband (TL-01) UVB phototherapy. Br J Dermatol. 1997 Jul;137(1):150-151. [PubMed]
4. Zachariae CO, Rossen K, Weissman K. An unusual severe case of subcorneal pustular dermatosis treated with cyclosporine and prednisolone. Acta Derm Venereol. 2000 Sep-Oct;80(5):386-387. [PubMed]
5. Bonifati C. Early but not lasting improvement of recalcitrant subcorneal pustular dermatosis (Sneddon-Wilkinson disease) after infliximab therapy: relationships with variations in cytokine levels in suction blister fluids. Clin Exp Dermatol. 2005 Nov;30(6):662-665. [PubMed]
6. Iobst W, Ingraham K. Sneddon-Wilkinson disease in a patient with rheumatoid arthritis. Arthritis Rheum. 2005 Dec;52(12):3771. [PubMed]
7. Butt A, Burge SM. Sneddon-Wilkinson disease in association with rheumatoid arthritis. Br J Dermatol. 1995 Feb;132(2):313-315. [PubMed]
8. Nagai H, Harada S. Subcorneal pustular dermatosis accompanied by seronegative arthritis. Acta Derm Venereol. 2002;82(4):318-319. [PubMed]
9. Scheinfeld NS, Worth R, Mallea J, Shookster L, Weinberg JM. Subcorneal pustular dermatosis developing in a patient with rheumatoid arthritis; rheumatoid, antimicrosomal, and antimitochondrial autoantibodies; and a goiter. SKINmed 2003:2;258-259. [PubMed]
10. Weiner S. Subcorneal pustular dermatosis and rheumatoid arthritis. Arthritis Rheum. 1981 Sep;24(9):1213-1214. [PubMed]
11. Undar L, Goze F, Hah MM. Subcorneal pustular dermatosis with seronegative polyarthritis. Cutis. 1988 Sep;42(3):229-32. [PubMed]
12. Roger H, Thevenet JB, Souteyrand P, Sauvezie B. Subcorneal pustular dermatosis associated with rheumatoid arthritis and raised IgA: simultaneous remission of skin and joint involvements with dapsone treatment. Ann Rheum Dis. 1990 Mar;49(3):190-191. [PubMed]
13. Tsuruta D, Matsumura-Oura A, Ishii M. Subcorneal pustular dermatosis and Sjogren's syndrome. Int J Dermatol. 2005 Nov;44(11):955-957. [PubMed]
14. Deleporte E, Colombel JF, Nguyen-Mailfer C, PyetteF, Cortot A, Bergoend H. Subcorneal pustular dermatosis in a patient with Crohn's disease. Acta Derm Venereol. 1992 Aug;72(4):301-302. [PubMed]
15. Saulsbury FT, Kesler RW. Subcorneal pustular dermatosis and systemic lupus erythematosus. Int J Dermatol. 1984;23:63-4. [PubMed]
16. Taniguchi S, Tsurata D, Kutsuna H, Hamada T. Subcorneal pustular dermatosis in a patient with hyperthyroidism. Dermatology. 1995;190(1):64-66. [PubMed]
17. Kohler LD, Mohrenschlager M, Worret WI, Ring J. Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in a patient with multiple sclerosis. Dermatology. 1999;199(1):69-70. [PubMed]
18. Cartier H, Plantin P, Leroy JP, Larzul JJ. Pyoderma gangrenosum, subcorneal IgA pustulosis and recurrent neutrophilic pleural and pulmonary diseases in a patient with IgA gammopathy. Ann Dermatol Venereol. 1995;122(3):97-101. [PubMed]
19. Scarpa R, Lubrano E, Cozzi R, et al. Subcorneal pustular dermatosis (Sneddon-Wilkinson syndrome): another cutaneous manifestation of SAPHO syndrome? Br J Rheumatol. 1997 May;36(5):602-603. [PubMed]
20. Wallach D. Subcorneal pustulosis and monoclonal gammapathies. Ann Med Interne. 1984;135(8):672-276. [PubMed]
21. Lutz ME, Daoud M, McEvoy M, Gibson L. Subcorneal pustular dermatosis: a clinical study of ten patients. Cutis. 1998 Apr;61(4):203-208. [PubMed]
22. Kasha EE Jr, Epinette WW. Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature. J Am Acad Dermatol. 1988 Nov;19(5 Pt 1):854-858. [PubMed]
23. Calista D. Subcorneal pustular dermatosis in a patient with AIDS. J Eur Acad Dermatol Venereol. 2003 Jul;17(4):478-479. [PubMed]
24. Villasante De La Puente A, Hormaechea Belderrain JA, Garcia Aguinaga ML, Vera Lopez E, Gilsanz Fernandez C. Pustulosis of Sneddon Wilkinson disease and multiple myeloma. An Med Interna. 2001 Jul;18(7):373-375. [PubMed]
25. Villey MC, et al. Apudoma and subcorneal pustular dermatosis (Sneddon-Wilkinson disease). Dermatology. 1992;185(4):269-271. [PubMed]
26. Otremba H. Sneddon-Wilkinson subcorneal pustulosis in pancreatic cancer. Dermatol Monatsschr. 1978 Mar;164(3):176-179. [PubMed]
27. Boyd AS, Stroud MB. Vesiculopustules of the thighs and abdomen. Subcorneal pustular dermatosis (Sneddon-Wilkinson disease). Arch Dermatol. 1991 Oct;127(10):1571, 1574. [PubMed]
28. Reed J, Wilkinson J. Subcorneal pustular dermatosis. Clin Dermatol 2000;18:301-313. [PubMed]
29. Sakkas LI, Chicanza IC, Platsoucas CD. Mechanisms of disease: the role of immune cells in the pathogenesis of systemic sclerosis. Nat Clin Pract Rheumatol. 2006 Dec;2(12):679-685. [PubMed]
30. Scheiferstein G, et al. Subcorneal pustular dermatosis of Sneddon-Wilkinson. A long-term immunologic case study. Arch Dermatol Res. 1984;276(1):65-68. [PubMed]
© 2009 Dermatology Online Journal



