Multicentric reticulohistiocytosis in a Malaysian Chinese lady: A case report and review of literature
Published Web Location
https://doi.org/10.5070/D34wm552ckMain Content
Multicentric reticulohistiocytosis in a Malaysian Chinese lady: A case report and review of literature
Felix Boon Bin, Yap MD (UNIMAS) MRCP (UK)
Dermatology Online Journal 15 (1): 2
Department of Dermatology, Sarawak General Hospital, Sarawak, Malaysia. woodzlamp@yahoo.comAbstract
A 36-year-old Malaysian woman with erosive arthritis presented with multiple asymptomatic skin colored papulonodules on the hands, elbows, knees, ears, and feet; many macules, papules, and plaques were photodistributed. Progressive, erosive arthritis began about 18 months after the onset of skin involvement. Initially the patient was diagnosed to have dermatomyositis due to her skin findings, but later proved to have multicentric reticulohistiocytosis based on the typical histopathological features of histiocytic multinucleated giant cells with eosinophilic ground glass cytoplasm on skin biopsy. Workup for associated diseases including malignancies was negative. Her skin lesions and joint pain responded to treatment with methotrexate and prednisolone.
Introduction
Multicentric reticulohistiocytosis is a rare systemic disease of unknown etiology characterized by mucocutaneous papulonodules and erosive arthritis. The cutaneous lesions consist of multiple reddish brown papules and nodules up to 2 cm in diameter, mainly involving the face and distal upper extremities. The arthritis preferentially involves the interphalangeal joints of the hands and can lead to joint destruction and deformities. Women outnumber men 3 to 1 [1]. The mean age of onset is in the fourth decade. Mycobacterium tuberculosis [2], autoimmune diseases and underlying malignancies are being considered as potential triggers [3]. Multicentric reticulohistiocytosis is reported to be associated with multiple medical conditions. Among the associated conditions, hyperlipidemia is reported in 30 to 58 percent of cases, a positive Mantoux test in 12 - 50 percent and underlying malignancies in 25 percent of cases [4]. The diagnosis is made by the typical histopathological findings of histiocytic multinucleated giant cells with eosinophilic ground glass cytoplasm. A patient with multicentric reticulohistiocytosis, likely the first in Malaysia is reported.
Clinical synopsis
A 36-year-old woman was seen in June 2007 for evaluation of multiple asymptomatic skin colored papulonodules on the hands (Fig. 1a), elbows, knees, ears (Fig. 1b) and feet for the past two years. Erythematous plaques along the photodistributed areas of the chest and back (Fig. 1c) were also noted.
 |
| Figure 1c |
|---|
| Figure 1c: Erythematous patches on the photodistributed back |
She had arthralgia and morning stiffness of the hands associated with asthenia, loss of appetite, and loss of 5 kg weight over 6 months. No proximal muscle weakness was noted.
With the clinical signs of photosensitivity and papular skin lesions resembling Gottron's papules, an initial impression of dermatomyositis was entertained.
 |
| Figure 2 |
|---|
| Figure 2: Well-circumscribed erosions on the distal interphalangeal joints of the index fingers |
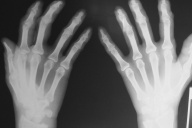
An extensive laboratory evaluation including complete blood count, erythrocyte sedimentation rate, serum chemistry profile, muscle enzymes, lipid profile, serum protein electrophoresis, antinuclear antibody, rheumatoid factor, viral hepatitis B and C serology, VDRL, HIV, Mantoux test, alpha fetoprotein, carcinoma embryonic antigen, Ca-125, fecal occult blood, urinalysis and thyroid function test were normal. Chest radiograph, abdominal and gynecological ultrasonography and cervical pap smear was also normal. Her hand X-rays showed well circumscribed erosions in the distal interphalangeal joints of the index fingers (Fig. 2).
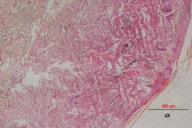
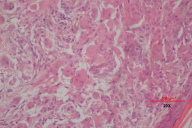
Skin biopsies were taken from a papule on the hand and a plaque on the back. The histopathological examination revealed dermal infiltrates consisting of multinucleated histiocytic giant cells with an eosinophilic 'ground glass' cytoplasm (Fig. 3a & 3b). Scattered lymphocytes were seen throughout the dermis. Immunohistochemistry was positive for CD68 and negative for S100. These features were consistent with multicentric reticulohistiocytosis.
 |
| Figure 4 |
|---|
| Figure 4: Worsening of the distal interphalangeal joint erosions in the index fingers with radial deviation of the distal phalanges. |
The patient began a regimen of oral methotrexate and prednisolone in September 2007. Prednisolone was slowly tapered down and stopped over a 4-month period. Her methotrexate was increased from 5 mg to 15 mg weekly. Her joint pain had disappeared with regression of the skin lesions, as had her photodistributed plaques. However, radial deviation of the proximal phalanx of both her index fingers was noted during her visit in June 2008. The X-ray showed worsening of her joint erosion in the distal interphalangeal joints (Fig. 4). Thus, prednisolone was restarted. Her Methotrexate was titrated up to 25 mg weekly. On her latest follow up in mid December 2008, she showed remarkable improvement in her skin lesions. The lesions on the ears and feet had disappeared and the ones on the hands, knees and elbows have become remarkable smaller (Fig. 5a & 5b). Her joint disease has remained stable with no further erosions noted.
 |  |
| Figure 5a | Figure 5b |
|---|---|
| Figure 5a. Regression of the papulonodules on the hands after 15 months of treatment. Figure 5b. Disappearance of papules on the helix of the right ear after 15 months of treatment. | |
Discussion
Multicentric reticulohistiocytosis is classified into Class II or non-Langerhans cell histiocytoses, characterized by local proliferation of resident mononuclear
phagocytes other than Langerhans cells [4]. This proliferation is believed to be due to the release of monokines, cytokines and other secretory products by the unregulated macrophage activation. These macrophage-derived cytokines have various pro-inflammatory actions including bone resorption and erosion of cartilage. The cytokines isolated include interleukin-1b, interleukin-6, interleukin-12, and tumor necrosis factor alpha [5].
Multicentric reticulohistiocytosis occurs predominantly in the Caucasian populations [1, 3]. A few cases were reported among Chinese, in Singapore [6], Hong Kong [7], and China [8]. It was never reported in Malaysia. It is believed that this is the first case of multicentric reticulohistiocytosis in Malaysia.
The onset of multicentric reticulohistiocytosis is usually insidious. The majority of patients present with initial articular signs and symptoms. The skin manifestations usually present months to years later, with a mean of three years [4]. Nevertheless, in some patients the cutaneous signs might precede or occur concurrently with the joint manifestations [1]. Interestingly the patient reported here followed the latter course, manifesting the skin signs 18 months before the articular symptoms.
The typical cutaneous manifestations consist of non pruritic flesh-colored to reddish brown yellow papules and nodules that may be found anywhere in the body, including the mucous membrane, but with predilection for the face and hands [3]. In one case, the nodules resembled neurofibroma [9]. The skin lesions may number a few to a few hundred. On the head, skin lesions mainly involve the ears, bridge of the nose, and scalp. On the hands, the dorsum and sides of the fingers are favored. Around the nailfolds, small tumefactions called 'coral beads' represent a typical clinical sign. Erythematous photo-distributed macules and papules are also reported [10]. The presence of the photo-distributed eruption and the presence of papulonodular lesions on the dorsum of the hands and interphalangeal joints, mimicking Gottron papules with periungual telangiectasia, might cause the confusion of multicentric reticulohistiocytosis with dermatomyositis [10, 11]. In this case, dermatomyositis was considered first because the incidence of dermatomyositis is higher, approximately 1:20,000 in Malaysia [12] compared to less than 300 reported cases of multicentric reticulohistiocytosis worldwide. The presence of erosive arthritis and the absence of muscular weakness usually point towards multicentric reticulohistiocytosis as the correct diagnosis.
Other conditions in the differential diagnosis include lepromatous leprosy, sarcoidosis, xanthomatosis, histiocytosis X, juvenile and adult xanthogranuloma, generalized eruptive histiocytoma, familial histiocytic dermatoarthritis, and neurofibromatosis [3]. The presence of skin manifestations on the face and hands with erosive arthritis usually differentiates multicentric reticulohistiocytosis from these diseases. The histiocytic diseases can usually be differentiated by histopathological and immunohistochemical studies. The presence of xanthalesma in a third of patients with multicentric reticulohistiocytosis [1] can cause confusion with familial dyslipidemia; the papulonodules may be mistakenly considered to be xanthomas. Lepromatous leprosy presenting with nodular lesions must always be considered in Malaysia as an item in the differential diagnosis. By proper examination including palpation for thickened nerves, slit skin smear examination, and skin biopsy, the diagnosis of leprosy can easily be made.
The arthritis in multicentric reticulohistiocytosis tends to be symmetrical, mainly affecting the interphalangeal joints of the hands [4]. The distal interphalangeal joints are most commonly affected (75%), followed by the knees, shoulders, wrists, hips, ankles, elbows and feet. Without proper treatment, the joint destruction is rapid, resulting in arthritis mutilans in half of the patients [1, 13]. Characteristically, at the interphalangeal joints, a disabling 'opera-glass' hand deformity is seen. Naturally, the disease will run its waxing and waning course until it burns out in 5 to 8 years.
Radiologically, joint erosion is evident, initially circumscribed and later spreading from the margin to involve the entire joint surface; this results in joint space widening, cartilage loss, and subchondral bone resorption [4]. Osteoporosis and periosteal new bone formation is notably absent, differentiating it from other inflammatory arthritis [13]. In the spine, bilateral, symmetrical erosions affecting the sacroiliac and costovertebral joints and bony ankylosis may develop without subchondral bony sclerosis [4].
The differential diagnoses for the joint manifestations include other forms of erosive polyarthritis, especially rheumatoid arthritis, psoriatic arthritis, erosive osteoarthritis and gouty arthritis. Multicentric reticulohistiocytosis is differentiated from rheumatoid arthritis by the presence of skin lesions, involvement of distal interphalangeal joints, and lack of juxtaarticular osteoporosis and joint space narrowing. The presence of psoriatic plaques, nail changes (especially thimble pitting), entheseal and periosteal new bone production, intra-articular bony ankylosis and an asymmetrical pattern of joint involvement differentiate psoriatic arthritis from multicentric reticulohistiocytosis. In erosive osteoarthritis, erosion is commonly sharply marginated in the central portion of the joint with the presence of marginal osteophytes and intra-articular bony ankylosis, the 'sea gull wing' pattern. Without these features, osteoarthirits can be confused with multicentric reticulohistiocytosis because both involve the distal interphalangeal joints and the papulonodules might be perceived as Bouchard's and Heberden's nodes. The presence of tophi and a non-demineralizing erosive arthritis with overhanging edges and reactive bony changes favors gouty arthritis.
Multicentric reticulohistiocytosisis is associated with multiple medical conditions. Malignancies are detected in a quarter to a third of cases [14, 15]. Breast and stomach malignancies are most commonly identified [4]. Others included cancer of the cervix, colon, lung, endometrium and ovary, lymphoma, leukemia, sarcoma, melanoma and cancer of unknown primary origin [3, 14, 16]. Multicentric reticulohistiocytosis usually antedates these malignancies in 75 percent of the cases and regresses on treatment of these cancers [15]. Thus, multicentric reticulohistiocytosis is controversially considered by some to be a paraneoplastic syndrome [3, 4]. Other associated diseases include hyperlipidemia, tuberculosis, preganancy, and autoimmune diseases. The patient presented here had extensive work up for these associated conditions. Fortunately, all the investigations were normal. Nevertheless, she will be vigilantly followed up for these diseases, especially underlying malignancies.
The characteristic dermatohistopathological findings of multicentric reticulohistiocytosis are the histiocytic, multinucleated eosinophilic ground-glass giant cells of foreign body type. These exhibit irregular size and shape reaching 50 to 100 μm and are distributed throughout the dermis [3]. They can also be found on synovial biopsy. They stain positively for PAS, Baker's acid hematein, and scarlet red O. Other inflammatory cells can also be found in the dermis, albeit in lesser numbers [4]. The overlying epidermis is mildly hyperkeratotic with some atrophy and flattening of the rete ridges [17]. Immunohistochemistry of the giant cells show a monocyte and macrophage origin, staining positively for CD68, HAM56, Mac387, alpha 1-antitrypsin, CD11b, CD11c, CD14, and CD15 [5]. S-100 and CD1a are negative, supporting a non-Langerhans cell histiocytic origin.
The disabling nature of this disease, particularly the destructive arthropathy, warrants aggressive management to prevent deformities and morbidities. However, the treatment of this disease is often complicated by waxing and waning, but it often spontaneous remits after 5 to 8 years. Various treatments have been used, with immunosuppressive agents having more success [3, 4]. Corticosteroids are useful for joint pain and have added advantage if combined with hydroxycholoquine for mild to moderate disease [18]. Methotrexate, cyclophosphomide, or chlorambucil used in combination with corticosteroids produced the best outcome in moderate to severe disease [4, 19]. It is suggested that the combination of methotrexate and prednisolone be considered for the arthritis and cyclophosphomide or chlorambucil added for the skin lesions [4]. Other treatments tried for this condition include cyclosporine and bisphosphonates [20, 21]. The use of tumor necrosis factor-alpha inhibitors, particularly infliximab, etanercept and adlimumab, showed conflicting results with most studies demonstrating promising outcomes [22, 23]. The rationale of using these medications is the demonstration of tumor necrosis factor-alpha in the involved synovium and the skin lesions. These medications are costly and may not be feasible in some countries unless more definitive benefit is shown. The patient presented responded to the combination of methotrexate and prednisolone.
In conclusion, a case of multicentric reticulohistiocytosis in a Malasian woman of Chinese descent is presented. The case is highlighted here due to its rarity among asians and is possibly the first reported case in Malaysia.
References
1. Barrow MV, Holubar K. Multicentric reticulohistiocytosis. A review of 33 patients. Medicine 1969; 48: 287- 305. [PubMed]2. Gold KD, Sharp JT, Estrada RG, Duffy J, Peterson DA. Relationship between multicentric reticulohistiocytosis and tuberculosis. JAMA 1977; 237: 2213- 4. [PubMed]
3. Tajirian AL, Malik MK, Robinson-Bostom L, Lally EV. Multicentric reticulohistiocytosis. Clin Dermatol 2006; 24: 486-92. [PubMed]
4. Trotta F, Castellino G, Monaco AL. Multicentric reticulohistiocytosis. Best Pract Res Clin Rheumatol 2004; 5: 759-72. [PubMed]
5. Gorman JD, Danning C, Schumacher HR, et al. Multicentric reticulohistiocytosis. Case report with immunohistochemical analysis and literature review. Arthritis Rheum 2000; 43: 930-938. [PubMed]
6. Giam YC, Ong BH. Multicentric reticulohistiocytosis. Ann Acad Med Singapore 1988; 17: 548-50. [PubMed]
7. Lau ST, Lee KC. Multicentric reticulohistiocytosis: a case report. J Hong Kong Med Assoc 1993; 45: 305-7.
8. Liu YH, Fang K. Multicentric reticulohistiocytosis with generalized systemic involvement. Clin Exp Dermatol 2004; 29: 373-6. [PubMed]
9. Hsu S, Ward SB, Le EH, Lee JB. Multicentric reticulohistiocytosis with neurofibroma-like nodules. J Am Acad Dermatol 2001; 44(2): 373-5. [PubMed]
10. Hsiung SH, Chan SF, Elinitsas R, Kolasinski SL, Schumacher HR, Werth VP. Multicentric reticulohistiocytosis presenting with clinical features of dermatomyositis. J Am Acad Dermatol 2003; 48: S11-4. [PubMed]
11. Mas A, Darwich E, Mascaro Jr JM, Herrero C. J Am Acad Dermatol 2008; 58: S2 AB98
12. US Census Bureau, International Data Base, 2004.
13. Gold RH, Metzger AL, Mirra JM, et al. Multicentric reticulohistiocytosis (lipoid dermatoarthritis). An erosive polyarthritis with distinctive clinical, roentgenographic and pathologic features. Am J of Roentgenol Radium Ther Nucl Med 1975; 124(4): 610-624. [PubMed]
14. Snow JL, Muller SA. Malignancy-associated multicentric reticulohistiocytosis: a clinical, histological and immunophenotypic study. Br J Dermatol 1995; 133(1): 7l-6. [PubMed]
15. Fam AG. Paraneoplastic rheumatic syndromes. Baillieres Best Pract Res Clin Rheumatol 2000; 14(3): 515-33. [PubMed]
16. Malik MK, Regan L, Robinson-Bostom L, Pan TD, McDonald CJ. Proliferating multicentric reticulohistiocytosis associated with papillary serous carcinoma of the endometrium. J Am Acad Dermatol 2005; 53(6): 1075-9. [PubMed]
17. Guillen C, Fortea JM, Serrano G,Martorell M, Cogollos E, Alegre V. Multicentric reticulohistiocytosis. Dermatologica 1984; 169(5): 311-7. [PubMed]
18. Carey RN, Blotzer JW, Wolfe ID, et al. Multicentric reticulohistiocytosis and Sjogren's syndrome. J Rheumatol 1985; 12(6): 1193-1195. [PubMed]
19. Franck N, Amor B, Ayral X, Lessana-Leibowitch M, Monsarrat C, Kahan A et al. Multicentric reticulohistiocytosis and methotrexate. J Am Acad Dermatol 1995; 33: 524-5. [PubMed]
20. Chalom EC, Rosenstein ED, Kramer N. Cyclosporine as a treatment for multicentric reticulohistiocytosis (letter). J Rheumatol 2000; 27: 556. [PubMed]
21. Adamopoulos IE, Wordsworth BP, Edwards JR, Ferguson DJ, Athanasou NA, Russell RGG. Bishosphonates inhibit bone resorption in multicentric reticulohistiocytosis. Bone 2006; 38(3): 65
22. Lovelace K, Kuykendall T, Crowson AN, Taylor JR. A case of multicentric reticulohistiocytosis treated with etanercept. J Am Acad Dermatol 2005; 52(3): P80.
23. Graves JE, Nunley K, Heffernan MP. Off label uses of biologics in dermatology: rituximab, omalizumab, infliximab, etanercept, adalimumab, efalizumab and alefacept (part 2 of 2). J Am Acad Dermatol 2007; 56(1): e55-79. [PubMed]
© 2009 Dermatology Online Journal