Extragenital bullous lichen sclerosus atrophicus
Published Web Location
https://doi.org/10.5070/D357m4h6nwMain Content
Extragenital bullous lichen sclerosus atrophicus
Irene Ballester, José Bañuls, María Pérez-Crespo, Ana Lucas
Dermatology Online Journal 15 (1): 6
Servicio de Dermatología Hospital General Universitario de Alicante, C/ Pintor Baeza s/n 03010, Spain. ibalnor@coma.esAbstract
Lichen sclerosus et atrophicus (LSA) is a rare, chronic, mucocutaneous disease of unknown etiology. Onset can occur in subjects of any age, but the condition is more prevalent in adult females around the time of menopause. In both sexes, the most common site of the lesions is the anogenital area. Bullous lichen sclerosus et atrophicus is an unusual form of the disease and the exact prevalence is not known. We describe a case of nongenital bullous LSA in a man.
Introduction
Lichen sclerosus et atrophicus (LSA) was first described by Hallopeau in 1887. Darier described the characteristic histological findings in 1892. Lichen sclerosus et atrophicus is a rare inflammatory disease of unknown etiology. It mainly affects post-menopausal women in the genital area. We describe a case of nongenital bullous LSA in a man.
Case report
An 80-year-old man consulted the dermatology clinic for a pruritic lesion on his back that had been present for two years. The patient attended the emergency room because the lesion, which had always been whitish, had become hemorrhagic and more raised in the previous 4-5 days. The patient reported that there had been no previous trauma.
 |
| Figure 3 |
|---|
| Figure 3. Appearance of the lesions after 3 weeks with treatment |
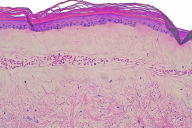
On physical examination the patient had a pearly white plaque with a hemorrhagic blister and follicular hyperkeratosis on the surface (Fig. 1). There were no other lesions in the genital area or in other sites. A biopsy was done and histological study revealed a sub-epidermal blister with marked edema of the papillary dermis, homogenization of collagen, atrophy of the epidermis, and extensive areas of hemorrhage (Fig. 2). All other complementary studies (complete blood count, biochemical parameters, and coagulation studies) were normal.
It was decided to start treatment with topical clobetasol propionate cream at 0.05 percent once daily for 3 weeks. At the return visit the hemorrhagic blister had resolved and an atrophic whitish plaque remained. After remaining inactive for 8 months, the plaque again became edematous and hemorrhagic, but to a lesser extent. Clobetasol propionate at 0.05 percent cream was prescribed again for two weeks and the lesion was much improved. To date, the plaque has remained stable for 20 months and no other new lesions have appeared.
Discussion
Lichen sclerosus et atrophicus is a relatively rare disease, the exact prevalence of which is not known. It predominates in women and may occur at any age. However, the maximum incidence occurs between the 5th and 6th decade of life and there is a second peak in girls between the ages of 8 and 13 years [1].
In both sexes it is most frequently found in the anogenital area. It is estimated that in 15-20 percent of cases there is also extragenital involvement. However, as in our patient, in 2.5 percent of cases it is found exclusively at an extragenital site [2]; the prevalence of extragenital LSA may be underestimated because it is often asymptomatic [3].
The underlying cause is unknown, but there seems to be a genetic susceptibility and a link with autoimmune mechanisms. The Koebner phenomenon occurs in lichen sclerosus—scarring or trauma may induce typical skin lesions of the disorder and extragenital lesions commonly occur in pre-existing scars and damaged areas [4].
Extragenital LSA is preferentially found on the trunk, neck, upper arms, flexor surfaces of the wrists, and forehead. Only very rarely are the palms of the hand, soles of the feet, face, scalp, and mouth affected. It is sometimes distributed following Blaschko lines [5]. Generalized forms have also been described [6].
In the first stages it presents as interfollicular, pearly, polygonal papules, which merge to form atrophic, sclerotic plaques. In more advanced stages, follicular hyperkeratosis and telangiectasias are seen. Hemorrhagic transformation often occurs and this appears to be due to basal cell degeneration that results in the dermal-epidermal union becoming fragile. Sometimes, as in our case, blister lesions are formed due to marked edema, with dilated vessels and hemorrhagic areas. When these blisters resolve, milia cysts may remain as residual lesions.
Histologically LSA has a characteristic pattern. Initially it presents as a superficial infiltrate with basal apoptosis. Hyperkeratosis, follicular occlusion, thinning of the epidermis and vascular alterations in the basal layer are seen in the epidermis. There is a large area of sub-epidermal edema with homogenization of collagen, sclerosis and dilation of the small vessels with hemorrhage. The elastic fibers are compressed by the edema and subsequently destroyed. A diffuse perivascular infiltrate of lymphocytes appears under the edema in the middle third of the dermis. As the edematous zone becomes bigger, the infiltrate becomes more disperse and usually less marked.
As opposed to the case of genital lesions, no increased risk of malignant transformation has been found in extragenital LSA.
There is no definitive treatment for LSA, although there are various therapeutic options to alleviate the symptoms. Numerous therapies have been used including topical corticosteroids, ointments containing estrogens or testosterone, retinoids, phototherapy, surgery and topical tacrolimus. Combined treatment of 0.1 percent tacrolimus ointment and PUVA may be a good option in extensive cases of lichen sclerosis or when other treatment options have failed [7]. In contrast to genital LSA, the extragenital form only requires treatment if it is very pruritic or anti-aesthetic in cases of severe sclerosis. The use of very potent corticosteroids such as clobetasol propionate at 0.05 percent has proved to be a safe and effective therapeutic option [8].
The interest of our case resides in the initial appearance of the nearly completely hemorrhagic appearance of the bullous lesion with only a very narrow whitish border, which made it difficult to diagnose. It is important to bear in mind this extragenital form of presentation of LSA in order to facilitate clinical diagnosis and thus reassure the patient without delay.
References
1. Smith YR, Haefner HK. Vulvar lichen sclerosus : pathophysiology and treatment. Am J Clin Dermatol. 2004; 5(2):105-25. [PubMed].2. Heymann WR. Lichen sclerosus. J Am Acad Dermatol. 2007 Apr; 56(4):683-4. [PubMed].
3. Meffert JJ, Davis BM, Grimwood RE. Lichen sclerosus. J Am Acad Dermatol. 1994 Oct; 31(4):671-3. [PubMed].
4. Powell JJ, Wojnarowska F. Lichen sclerosus. Lancet. 1999 May; 353(9166):1777-83. [PubMed].
5. Choi SW, Yang JE, Park HJ et al. A case of extragenital lichen sclerosus following Blaschko's lines. J Am Acad Dermatol. 2000 Nov; 43 (5 Pt 2):903-4. [PubMed].
6. Silverio AD, Serri F. Generalized bullous and haemorrhagic lichen sclerosus et atrophicus. Marked improvement with ACTH. Br J Dermatol. 1975 Aug; 93(2):215-7. [PubMed].
7. Valdivielso-Ramos M, Bueno C, Hernanz JM. Significant Improvement in Extensive Lichen Sclerosus with Tacrolimus Ointment and PUVA. Am J Clin Dermatol. 2008; 9(3):175-9. [PubMed].
8. Kim YJ, Lee ES. Case of sequentially occurring lesions of facial lichen sclerosus following the lines of Blaschko. J Dermatol. 2007 Mar; 34(3):201-4. [PubMed].
© 2009 Dermatology Online Journal