Dermatoscopy in the diagnosis of tinea nigra
Published Web Location
https://doi.org/10.5070/D30g09t0dfMain Content
Dermatoscopy in the diagnosis of tinea nigra
Marcus Henrique de S B Xavier MD, Lúcia Helena S Ribeiro PhD, Hélio Duarte PhD, Giani Saraça PhD, Ângela Cristina L Souza
MD
Dermatology Online Journal 14 (8): 15
Universidade Federal Fluminense, Hospital Universitário Antônio Pedro, Serviço de Dermatologia, Niterói, Rio de janeiro, Brazil.
marcus_hx@hotmail.comAbstract
Tinea nigra is an asymptomatic superficial fungal infection caused by Phaeoannelomyces werneckii, generally affecting the skin of the palms and characterized by deeply pigmented macular non-scaly patches. These lesions are quite characteristic. However, they can be misdiagnosed as a malignant melanoma or a junctional melanocytic nevus and unnecessary biopsies may be performed. Thus, dermoscopy is a fast, useful, clinical adjunctive tool in differentiating tinea nigra from melanocytic lesion.
Clinical synopsis
A 10-year-old caucasian boy presented with a 3-month history of a slow-growing pigmented lesion on his left palm. He denied pruritus or pain. He had no relevant history of trauma and his medical history was dislipidemic controlled only with diet. He frequently played in gardens and beaches.
 |  |
| Figure 1 | Figure 2 |
|---|
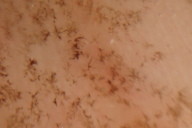
Physical examination revealed a 3cm brown macule (Fig. 1) with a minimum of desquamation and well-delimited borders (Fig. 2). The left axilary and upper member lymph nodes were not palpable.
 |  |
| Figure 3 | Figure 4 |
|---|
Dermatoscopy examination of the palm lesion showed a homogeneous nonmelanocytic pigmented pattern with spicules that did not follow the dermatoglyphic lines in the irregular macule. (Figs. 3 & 4)
 |
| Figure 5 |
|---|
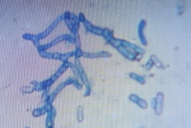
Potassium hydroxide preparation of lesional skin scrapings demonstrated numerous pigmented septate hyphae, with varying diameter (Fig. 5). The child was treated with 1 percent Isoconazole cream twice a day for 3 weeks with complete resolution.
After 21 days the culture on Sabouraud agar at room temperature showed moist black colonies, which were identified as Phaeoannelomyces werneckii.
There was no recurrence upon examination 3 months later.
Comments
Tinea nigra or keratophytosis negra consists of a chronic fungal infection of the stratum corneum of the epidermis whithout inflammation by Phaeoannelomyces werneckii. In Venezuela, there are case reports of tinea nigra caused by Stenella araguata, autochthonous in that country [1]. Tinea nigra has predilection for tropical and subtropical regions in Asia, Africa, and Central and South America, but there have been cases in the North America [2]. P. werneckii is a saprobic fungus living alone in the following environments: soil, plants, beach, sand, air and decomposing fish. This mycosis occurs more often in children and adolescents, particularly girls [3].
The period of incubation of tinea nigra varies from two to seven weeks. It typically presents as unilateral, asymptomatic sharply demarcated of one or more brown or black macules, wich can join and envolve centrifugally growing to between one and five centimeters. There is minimum desquamation and well delimited borders localize mainly on the palmar regions and the fingers, but rarely on the plants of the feet, dorsal aspects of the hands, cervical and back region [4]. Potassium hydroxide preparation of lesional skin scrapings of the lesion show numerous pigmented septate hyphae. Cultures on Sabouraud agar at room temperature show slow-growing, moist and shiny black colonies [5]. They are composed of oval to spindle-shaped cells, many of them with a central cross wall. These lesions are quite characteristic. However, they can be misdiagnosed as a malignant melanoma or a junctional melanocytic nevus and unnecessary biopsies may performed [6]. Thus, dermoscopy is a fast, useful, clinical adjunctive tool in differentiating tinea nigra from melanocytic lesion [7, 8]. Gupta et al. [9] originally described the dermatoscopic findings of tinea nigra as a nonmelanocytic pattern of pigmented spicules, thus aiding in differentiating this lesion from a pigmented lesion that should be biopsied. Treatment could be performed with topical antifungal therapy, although keratolytic agents have also been used [6]. Complete resolution typically occurs with two weeks of treatment. There is a report of successful treatment with oral itraconazole [9]. There is rarely any recurrence [2].
References
1. Perez C, Colella MT, Olaizola C, et al. Tinea Nigra: Report of twelve cases in Venezuela. Mycopathologia. 2005; 160:235-238. PubMed2. Moreira VMS, Santos VLC, Carneiro SCS, et al. Ceratofitose Negra. An Bras Dermatol. 1993; 58(5):281-5. [No PMID]
3. McKinlay JR, Barret TL, Ross EV. Picture of the month. Tinea Nigra. Arch Pediatr Adolesc Med. 1999; 153:305-306. PubMed
4. Diniz, LM. Study of nine observed cases of Tinea Nigra in Greater Vitória (Espírito Santo state, Brazil) over a period of five years. An Bras Dermatol. 2004; 79(3):305-310. [No PMID]
5. Pegas JR, Criado PR, Lucena SK, et al. Tinea Nigra: Report of two cases in infants. Pediatric Dermatology. 2003; 4:315-317. PubMed
6. Hall J, Perry VE. Tinea Nigra palmaris: differentiation from malignat melanoma or junctional nevi. Cutis. 1998; 62:45-46. PubMed
7. Smith SB, Beals SL, Elston DM, Meffert JJ. Dermatoscopy in the diagnosis if Tinea Nigra Plantaris. Cutis. 2001; 68:377-380. PubMed
8. Zalaudek I, Giacomel J, Cabo H, Di Stefani A, Ferrara G, Hofmann-Wellenhof R, Malvehy J, Puig S, Stolz W, Argenziano G. Entodermoscopy: a new tool for diagnosing skin infections and infestations. Dermatology. 2008; 216(1):14-23. PubMed
9. Gupta G, Burden AD, Shankland GS, et al. Tinea Nigra secondary to Exophiala werneckii responding to itraconazole. Br J Dermatol. 1997; 137:483-484. PubMed
© 2008 Dermatology Online Journal

