Noninvoluting congenital hemangioma
Published Web Location
https://doi.org/10.5070/D38kf57566Main Content
Noninvoluting congenital hemangioma
Jennifer A Stein MD PhD, Noushin Heidary MD, Melissa Pulitzer MD, Julie V Schaffer MD, Paula North MD PhD
Dermatology Online Journal 14 (5): 7
Department of Dermatology, New York UniversityAbstract
An 8-year-old boy presented with a lifelong history of a vascular mass overlying his right mandible with central coarse telangiectases and peripheral pallor. Histopathologic examination showed a proliferation of blood vessels in the dermis. Ultrasound examination identified a mix of high- and low-flow vessels within the lesion. These findings were consistent with a noninvoluting congenital hemangioma, a rare vascular tumor that is fully formed at birth and grows proportionately with the patient without subsequent regression.
Clinical synopsis
The patient presented to the Charles C. Harris Skin and Cancer Pavilion for evaluation of a vascular mass on his right mandible. His mother noticed the prominent blood vessels, bluish coloration, and swelling in this area during the first few months of his life. Over time, the lesion had enlarged proportionally with the patient's growth and had become more prominent within the past year. There was no family history of vascular lesions. The patient had no other medical problems and was not taking any medications. A review of symptoms was negative.
Physical examination
Overlying the right mandible was a warm, soft, partially-compressible mass that measured 2.5- x 1.5-cm in diameter. The lesion was light blue-violet in color, with central coarse telangiectases and peripheral pallor.
 |  |
| Figure 1 | Figure 2 |
|---|
Laboratory data
Ultrasound evaluation of the lesion showed a markedly hyperemic dermal and subcutaneous mass. Color doppler evaluation of several round and tubular anechoic structures within the mass demonstrated both low-resistance, high-velocity arterial flow and venous flow. An arterial feeder vessel was identified in the deeper subcutaneous soft tissues.
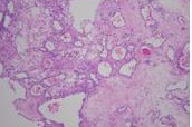
Histopathology
There is a nodular proliferation of thin-walled blood vessels of various calibers within the deep reticular dermis and subcutis. GLUT1 staining was negative.
Comment
The noninvoluting congenital hemangioma (NICH) is a rare vascular tumor that is fully formed at birth, grows proportionally with the patient or expands slightly over time, and does not regress [1, 2]. This growth pattern distinguishes NICH from the infantile hemangioma (IH), which is a common vascular tumor that appears within the first few months of life, grows rapidly during the first 6 months to 1 year, and subsequently regresses slowly over several years [3]. The other major subtype of congenital hemangioma is the rapidly-involuting congenital hemangioma (RICH), which is also fully formed at birth but completely regresses within the first 6 months to 1 year of life [4]. Noninvoluting congenital hemangioma and RICH were first recognized as distinct entities in 2001, based upon their characteristic growth patterns as well as a lack of immunoreactivity for the glucose transporter-1 protein (GLUT1) [1, 2], a sensitive and specific marker for IHs [5]. This protein is not detectable in the blood vessels of normal skin or in most other types of vascular tumors but is highly expressed in endothelia at sites of blood-tissue barriers, which include the brain and placenta.
Clinically, NICH presents as a round or oval mass that is pink-to-blue-violet in color, with central coarse telangiectases and peripheral pallor. The lesions are warmer than is the surrounding skin, and large draining veins sometimes can be observed at the periphery. The lesions of NICH are found most often on the head and neck and commonly overly the mandible or occur on the extremities near a joint [1, 2, 6, 7]. On histopathologic examination, NICH and IH have similar appearances. Both are composed of lobules of proliferating capillaries within the dermis and sometimes involve the subcutis. The vessels are thin-walled channels that are lined by plump endothelial cells and one or more layers of pericytes. However, some authors have described subtle histpathologic features that suggest a diagnosis of NICH. These changes include the presence of dilated veins and sometimes arteries between the vascular lobules, dermal arteriovenous microfistulae, a large stellate vessel in the center of the lobules, hobnailing of endothelial cell nuclei, and thin basement membranes [1, 2, 6, 7]. Both NICH and IH in the proliferative phase are fast-flow lesions when examined with ultrasound analysis and magnetic resource imaging (MRI).
A recent retrospective study attempted to determine imaging characteristics that can help to differentiate NICH from IH [8]. Sonographically visible vessels (veins or arteries) represented the only feature that was appreciably more common in NICH (72%, 13/18 lesions) than it was in IH (15%, 4/26 lesions). Evidence of heterogeneity and calcifications with ultrasound analysis also were suggestive of a diagnosis of NICH. With MRI, NICH and IH are similar in appearance, and demonstrate hyperintensity on T2-weighted sequences and flow voids [8]. The lack of GLUT1 staining in NICH and RICH suggests that they are biologically distinct from IH. The pathogenesis of the former lesions has not been elucidated, whereas IH are postulated to arise from embolized placental cells or angioblasts that differentiate toward a placental microvascular phenotype [3]. However, there have been reports of infants with a RICH or NICH and a coexistent IH as well as patients with a congenital hemangioma that began to regress rapidly then ceased to involute, and left a residual fast-flow tumor typical of a NICH. These observations imply that links exist between RICH, NICH, and IH [9]. It is important to distinguish NICH from IH because of the differences in their management. Congenital hemangiomas should be observed for 18 months to monitor for regression. If the lesion appears to be noninvoluting, it can be examined by ultrasound to confirm the presence of fast flow; GLUT1 staining of a biopsy specimen also can be considered. Treatment of NICH is surgical excision. Some patients may require arterial embolization to control bleeding, but most lesions can be excised without complications or recurrence [1, 6].
References
1. Enroljas O, et al. Noninvoluting congenital hemangioma: a rare cutaneous vascular anomaly. Plast Reconstr Surg 2001; 107:16472. North PE, et al. Congenital nonprogressive hemangioma: a distinct clinicopathologic entity unlike infantile hemangioma. Arch Dermatol 2001; 137:1607
3. Bruckner A, Frieden I. Infantile hemangiomas. J Am Acad Dermatol 2006; 55:671
4. Berenguer B, et al. Rapidly involuting congenital hemangioma: clinical and histopathologic features. Pediatr Dev Pathol 2003; 6:495
5. North PE, et al. GLUT1: a newly discovered immunohistochemical marker for juvenile hemangiomas. Hum Pathol 2000; 31:11
6. Krol A, MacArthur CJ. Congenital hemangiomas: rapidly involuting and noninvoluting congenital hemangiomas. Arch Facial Plast Surg 2005; 7:307
7. Matulich J, et al. Case of non-involuting congenital haemangioma. Australas J Dermatol 2005; 46:165
8. Gorincour G, et al. Imaging characteristics of two subtypes of congenital hemangiomas: rapidly involuting congenital hemangiomas and non-involuting congenital hemangiomas. Pediatr Radiol 2005;35:1178
9. Mulliken JB, Enjolras O. Congenital hemangiomas and infantile hemangioma: missing links. J Am Acad Dermatol 2004; 50:875
© 2008 Dermatology Online Journal

