Epidermodysplasia verruciformis
Published Web Location
https://doi.org/10.5070/D36715108zMain Content
Epidermodysplasia verruciformis
Christopher M Hunzeker MD, Anthony C Soldano MD, Steven Prystowsky MD
Dermatology Online Journal 14 (3): 2
Department of Dermatology, New York UniversityAbstract
A 29-year-old woman presented for evaluation of an ulcerated nodule on her right temple in the presence of numerous additional scaly papules, plaques, and seborrheic keratosis-like lesions that were distributed on her forehead, frontal scalp, and temples. Further examination showed pityriasis rosea-like lesions on her neck, back, and arms and verruca plana-like lesions on the dorsa of the hands and forearms. A biopsy specimen of the ulcerated nodule showed a nodular basal-cell carcinoma. Two additional biopsy specimens from her forehead showed one invasive and one in-situ squamous-cell carcinoma. Both biopsy specimens demonstrated histopathologic evidence of epidermodysplasia verruciformis.
Clinical synopsis
A 29-year-old woman presented to Bellevue Hospital Center Dermatology Clinic in January 2007 for evaluation and treatment of an ulcerated nodule on her right temple that had enlarged rapidly over several months. The lesion bled on several occasions after minor trauma and was similar to a cancer of her left frontal scalp that was surgically excised in Mexico 3 years previously. At the time of presentation it also was apparent that the patient had numerous red and brown lesions on her forehead and temples. The lesions had been increasing in number for 5 years and were intermittently pruritic. The patient took no medications and denied a family history of skin cancer or personal history of radiation exposure. A review of systems was negative. She was born in Mexico City and moved to Guerrero, Mexico at age 5. In Guerrero, she received intense sun exposure on a daily basis until the age 24 when she and her husband moved to New York.
Physical examination
 |
| Figure 1 |
|---|
On the right temple, just lateral to the brow, was a 1.5-cm x 1.5-cm x 1.5-cm, ulcerated, exophytic nodule. Scattered on her forehead, frontal scalp, and temples were pink and red-brown, focally hyperpigmented papules and thin plaques as well as several dark brown macules and verrucous papules, which demonstrated on examination with a dermatoscope, sharp borders, comedo-like openings, and milia-like cysts. On the left frontal scalp was an oval, 7-cm x 4-cm, fibrotic, depressed plaque with alopecia. On her upper back, neck, and extensor aspects of the upper extremities were numerous pink macules, papules, and thin plaques. There were no findings on the palms, soles, or oral mucosa.
Laboratory data
Radiographs of the mandible, skull, ribs, and vertebral column were normal.
Histopathology
 |  |
| Figure 2 | Figure 3 |
|---|
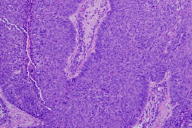
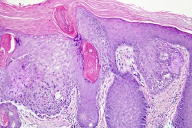
In one specimen, there is full thickness epidermal atypia with parakeratosis extending down follicular epithelium and focal infiltration into the underlying dermis. In the adjacent epidermis there are keratinocytes in the spinous and granular layers with prominent blue-gray granules within their cytoplasm. In a second specimen, emanating from an ulcerated epidermis is a basaloid proliferation of cells with peripheral palisading of the nuclei. There are mitotic figures and apoptotic cells.
Comment
Epidermodysplasia verruciformis (EV) is rare, autosomal recessive genodermatosis that is characterized by susceptibility to infection with a variety of human papillomavirus (HPV) genotypes that are considered to be innocuous for the general population [1]. Patients develop cutaneous lesions in early childhood, and an appreciable proportion of these patients progress to develop non-melanoma skin cancers as early as the third decade of life. Epidermodysplasia verruciformis is associated with nonsense mutations in two adjacent genes, EVER1 and EVER2, which are located on chromosome 17q25 [1]. The genetic mutations render individuals susceptible to infection with HPV5, 8, 9, 12, 14, 15, 17, 19-25, 36-38, 47, and 49. These HPV types, which are referred to as EV-HPV types, are ubiquitous and harmless to healthy, unaffected individuals [2, 3]. Individuals with EV are not at increased risk for bacterial, fungal, or other viral infections nor are they abnormally susceptible to genital HPV genotypes [1].
Cutaneous lesions in EV are highly polymorphic. Patients often first develop persistent verruca plana-like lesions. Over time, they may also develop pityriasis versicolor-like macules; pink, red or brown, scaly papules and plaques; seborrheic keratosis-like lesions; and eventually actinic keratoses and non-melanoma skin cancers [4]. Lesions are observed predominantly in sun-exposed areas, especially the forehead, neck, and dorsa of the hands. Non-melanoma skin cancers, primarily squamous-cell carcinomas (SCCs), have been reported to occur in greater than 50 percent of patients with EV [5]. While some authors report a rather indolent course for these tumors, others have documented extremely aggressive and metastatic carcinomas, which included cases that resulted in death [5, 6]. Oncogenic EV-HPV types, namely HPV5 and HPV8, have been isolated in upwards of 90 percent of EV-associated SCCs [7]. Ultraviolet radiation exposure appears to be a necessary co-carcinogen in the pathogenesis of EV-associated malignant conditions. Ultraviolet radiation may directly activate certain oncogenic HPV genotypes and/or activate viral replication indirectly by inducing local or systemic immunosuppression [8, 9]. A dysfunction in the p53 gene also appears to play a role in EV carcinogenesis [10]. Sun avoidance and sun protection are of paramount importance for EV patients.
Morbidity and mortality may be avoided by early recognition of the disease, sun avoidance, monitoring by a dermatologist, and treatment of premalignant and malignant lesions. Surgical excision is the appropriate treatment for invasive carcinomas; however, adjunctive methods may be employed to treat premalignant lesions and, thus, minimize the number of surgeries needed. Case reports have claimed effective treatment of EV with the combination of acitretin and interferon alfa-2a and also with topical 5-aminolevulinic acid and photodynamic therapy [11, 12]. There is one case report claiming successful treatment of EV with imiquimod.
Our patient presented with an ulcerated BCC. While BCCs have been described in EV, they are seen much less frequently than are SCCs. One study of 62 EV patients showed a ratio of 16 SCCs to 1 BCC [7]. The numerous pink and red-brown, focally hyperpigmented papules and plaques on her forehead appeared clinically consistent with pigmented BCCs, and, thus, radiographs of her skull, mandible, ribs, and spine were obtained to rule out Gorlin syndrome. It was the histopathologic changes in subsequent forehead biopsy specimens and the distribution of lesions limited to chronically sun-exposed sites that led to the diagnosis of EV. Our patient has undergone surgical excision of the ulcerated nodular BCC and is set to begin a course of topical 5-fluorouracil to reduce the number of clinically premalignant and in-situ SCCs on her forehead and temples.
References
1. Ramoz N, et al. Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat Genet 2002; 32:5792. Antonsson A, et al. Prevalence and type spectrum of human papillomaviruses in healthy skin samples collected in three continents. J Gen Virol 2003; 84:1881
3. Harwood CA, Proby CM. Human papillomaviruses and non-melanoma skin cancer. Curr Opin Infect Dis 2002; 15:101
4. de Oliveira WRP, et al. Clinical aspects of epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol 2003; 17:394
5. de Oliveira WRP, et al. Skin cancer in epidermodysplasia verruciformis patients from Brazil. J Eur Acad Dermatol Venereol 2006; 20:1133
6. Jablonska S. Epidermodysplasia verruciformis. In: Friedman RJ, et al, eds. Cancer of the Skin. Philadelphia: W.B. Saunders,1991: 101
7. Harris AJ, et al. A novel human papillomavirus identified in epidermodysplasia verruciformis. Br J Dermatol 1997: 136:587
8. Akgul B, et al. UV-B irradiation stimulates the promoter activity of the high-risk, cutaneous human papillomavirus 5 and 8 in primary keratinocytes. Arch Virol 2005; 150:145
9. Termorshuizen F, et al. Sunlight exposure and (sero) prevalence of epidermodysplasia verruciformis-associated human papillomavirus. J Invest Dermatol 2004; 122:1456
10. Padlewska K, et al. Mutation and abnormal expression of the p53 gene in the viral skin carcinogenesis of epidermodysplasia verruciformis. J Invest Dermatol 2001; 117:935
11. Anadolu R, et al. Treatment of epidermodysplasia verruciformis with a combination of acitretin and interferon alfa-2a. J Am Acad Dermatol 2001; 45:296
12. Karrer S, et al. Epidermodysplasia verruciformis treated using topical 5-aminolevulinic acid photodynamic therapy. Br J Dermatol 1999; 140:935
© 2008 Dermatology Online Journal

