Longitudinal leukonychia in Hailey-Hailey Disease: a sign not to be missed
Published Web Location
https://doi.org/10.5070/D36x16x4z0Main Content
Longitudinal leukonychia in Hailey-Hailey Disease: a sign not to be missed
Rajesh Kumar MD1, Vijay Zawar MD2
Dermatology Online Journal 14 (3): 17
1. Jagjivan Ram Hospital, Mumbai, India. rkderm@gmail.com2. Skin Disease Centre, Nashik, India
Abstract
A 54-year-old male presented with a painful, erythematous, fissured plaque involving the left groin and adjacent scrotal skin. In addition, he exhibited white longitudinal bands and ridges on his fingernails, more prominent on thumb nails. Skin biopsy from the left groin confirmed the diagnosis of chronic familial benign pemphigus (Hailey-Hailey disease). To the best of our knowledge, this is the first case report from India in which we have described nail involvement in Hailey-Hailey disease.
Introduction
Chronic familial benign pemphigus, Hailey-Hailey disease (HHD), is a rare, autosomal dominant disorder with incomplete penetrance. It is characterized by intraepidermal blistering resulting in recurrent vesicular eruptions mainly localized to the flexural areas of the body, such as groin, axilla, neck, and periumblical area [1, 2, 3]. Being a dominant autosomal disorder, it is often seen in siblings and extended family members [4, 5]. Hailey-Hailey Disease can rarely involve the mucosa of the esophagus [6], oral cavity [7], conjunctiva [8] and vagina [9]. Nail involvement was not much appreciated before Burge described it in her study of 38 patients, with an incidence as high as 70 percent (27 of 38) [1]. She noted that the nail involvement is usually asymptomatic and is often missed if not specifically looked for [3]. The significance of this finding was also stressed by Kirtschig et al. [10]. We highlight this important nail sign in HHD.
Case report
 |
| Figure 1 |
|---|
| Figure 1. Showing typical plaque involving the left side of groin |
A 54-year-old male dentist presented with a painful, erythematous, fissured plaque involving the left groin and adjacent scrotal skin (Fig. 1), present for the last ten years. The lesion was intermittently painful especially during the summer months, which restricted his mobility. He had been treated at different centers with various medications including topical antifungal creams, lotions, and powders. His various treatments included clotrimazole and miconazole; topical antibiotics such as framycetin, fucidic acid, mupirocin, and sisomicin; and systemic antibiotics including erythromycin, roxithromycin, cephadroxyl, and ampicillin-cloxacillin. None of these had given any significant improvement.
 |  |
| Figure 2a | Figure 2b |
|---|---|
| Figure 2a. Showing involvement of finger nails Figure 2b. Showing longitudinal leukonychia and ridging | |
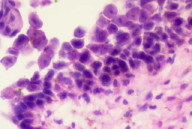
On examination, in addition to plaque involving the left groin he had asymptomatic white longitudinal bands on all his fingernails, but most prominently over the thumbs (Fig. 2a). Closer inspection of the thumb nails revealed flat longitudinal bands in addition to a few ridges (Fig. 2b). Affected nails were non-fragile and did not show distal notching. In addition to being white, parts of the nail also showed longitudinal ridging. His toe nails, palms, soles, and mucosae were uninvolved. There was no evidence of any associated systemic disorder or any other cutaneous disease, including Darier's disease. There was neither a relevant drug history nor was there a past or family history of psychiatric illness.
Careful family history revealed that his mother, elder brother, and younger sister had a similar kind of cutaneous disease affecting both axillae and groins with a history of exacerbation in the summer months. In spite of our best effort, his brother and sister could not be contacted for detailed examination. His mother died a few years ago due to old age. Examination of his son revealed subtle longitudinal white bands involving the 5th and middle fingers, but no skin eruptions.
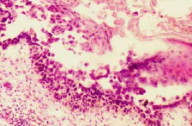
Repeated skin scrapings for fungus were negative. Other investigations including complete blood counts, blood sugar, urinalysis, liver function tests, and serological tests for syphilis and HIV antibodies were negative. A skin biopsy taken from the edge of the plaque in the left groin showed spongiosis, partial acantholysis with intraepidermal cleft formation and the typical "dilapidated brick wall appearance" of the epidermis, thus confirming a diagnosis of HHD (Figs. 3a & 3b). Direct immunoflurescence was negative.
 |  |
| Figure 3a | Figure 3b |
|---|---|
| Figure 3a. 10X Histopathology of skin lesions Figure 3b. 40X Histopathology showing partial acntholysis | |
He was treated by combination of sodium fusidate and betamethasone dipropionate 0.05 percent cream as local application twice a day for three weeks; the plaque completely resolved leaving post-inflammatory hyperpigmentation. There was no recurrence for next six months. With onset of the next summer, he developed a recurrence which was rapidly controlled by the same topical medication. The nail findings remained unchanged during and after treatment.
Discussion
Hailey-Hailey disease (HHD) is a chronic disease with exacerbations and remissions [1, 2, 3]. It is often described as "Benign Pemphigus" since it is not life-threatening as is pemphigus vulgaris. However, it causes significant morbidity. The nail involvement in HHD has been described in one study and one case report [3, 10]. In our case of HHD, the nail involvement was asymptomatic and familial; it mainly affected the thumb nails. During the period of observation over two years, there was no change in the nail signs during treatment and regression of the cutaneous eruption in the groins. It may be likely that the nail lesions are long-lasting and do not correspond to the disease activity. Hence, these do not seem to have prognostic importance. Thus, nail involvement in our case was seen in concordance with that observed by Burge [3]. A similar observation of longitudinal leukonychia in father and son was described by Kirtschig et al [10]. The nail involvement in our case was not bothersome for the patient. Our patient and his son did not insist on its treatment nor did they consent to nail biopsy. It will be important to watch for signs of development of the typical erosive plaques in the son; his mild nail changes may be an early sign of the disease. We informed the patient about the possibility of development of HHD in his son at a later date.
The pathogenesis of the nail involvement is unexplained. Some investigators in the past noted the nail changes, but they considered HHD to be a vesicular variant of Darier's disease and attributed the nail changes to Darier's disease [12]. However, in patients with Darier disease, apart from longitudinal white bands, they often have other typical signs such as notching of the free end of the nail, nail fragility, painful splitting, red lines, or alternate red and white lines [13]. Moreover, nail abnormalities are generally symptomatic in Darier disease, unlike HHD [13]. Although HHD and Darier disease and distinct entities, their occurrence in the same patients has been reported [14]. Nail changes can provide a supporting clue in a suspected case of HHD where there are insufficient clinical signs or histopathology is not possible. Moreover, these could serve as a screening test for the other family members in whom there is no overt HHD. It might be possible that nail changes are the earliest signs of the disease and their observation may help identify family members who are likely to develop HHD.
ACKNOWLEDGEMENTS: The authors would wish to acknowledge Dr. Shanker Sawant of Nair Hospital, Mumbai and Dr. (Mrs.) Aruna Madan of Jagjivan Ram Hospital, Mumbai in providing us the histopathology of the lesions and photomicrograph.
References
1. Burge SM. In: Textbook of Dermatology: Editors: Champion RH,Burton JL, Burns DA, Breathnach SM, 6th edition, Blackwell Science London, 1998; Chapter 40, Bullous Eruptions. 1844-18472. Hailey H,Hailey H. Familial benign chronic pemphigus. Arch Dermatol syphilol 1939; 39:679- 685
3. Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol 1992; 126: 275-282. PubMed
4. Sehgal VN, Jain S. Chronic familial benign pemphigus. J Dermatol 1994; 21: 382-388 PubMed
5. Cullen DR. Genetic features of familial benign pemphigus. Br J Dermatol 1965; 77: 20-23 PubMed
6. Kahn D, Hutchinson E. Esophageal involvement in familial benign chronic pemphigus. Arch Dermatol 1974; 109: 718-719 PubMed
7. Botvinick I. Familial benign pemphigus with oral mucous membrane lesions. Cutis 1973; 12: 371-373
8. Oguz O, Gokler G, Ocakoglu O, et al: Conjunctival involvement in familial chronic benign pemphigus (Hailey- Hailey disease). Int J Dermatol 1997; 36(4): 282-285 PubMed
9. Vaclavinkova V, Neumann E. Vaginal involvement in familial benign chronic pemphigus (morbus Hailey Hailey). Acta Derm Venereol (Stoch) 1982; 62: 80-81 PubMed
10. Kirtschig G, Effendy I, Happle R. Leukonychia longitudinalis as the primary symptom of Hailey-Hailey disease. Hautarzt. 1992 ;43(7):451-452. PubMed
11. Dhitavat J, Fairclough RJ, Hovnavian A, Burge SM. Calcium pumps and keratinocytes: lessons from Darier's disease and Hailey-Hailey Disease. Br J Dermatol. 2004; 150(5):821-828. PubMed
12. Ronchese F. The nail in Darier's disease. Arch Dermatol 1965; 91: 617-618 PubMed
13. Ellis FA. Vesicular Darier's disease (So called benign familial pemphigus). A variant of Darier's disease. Arch Dermatol Syphiliol 1950; 61: 715-736 PubMed
14. Nicolis G, Tosca A, Marouli O, Stratigos J: Keratosis follicularis and familial benign Pemphigus in the same patient. Dermatologica 1979; 159: 346-51; PubMed
© 2008 Dermatology Online Journal

