Epidermodysplasia verruciformis in the setting of HIV infection
Published Web Location
https://doi.org/10.5070/D38wf0515gMain Content
Epidermodysplasia verruciformis in the setting of HIV infection
Peter Chien Jr. MD PhD, Hideko Kamino MD, Ruth F Walters MD, Karla Rosenman MD, Miriam K Pomeranz MD, Miguel Sanchez MD
Dermatology Online Journal 14 (10): 1
Department of Dermatology, New York UniversityAbstract
A 56-year-old man with human immunodeficiency virus infection presented with pink-to-hypopigmented, thin, flat-topped papules coalescent to plaques on the trunk and extremities for five years. The histopathologic findings were consistent with flat warts resembling epidermodysplasia verruciformis. Typically an inherited condition, this entity has also been observed in the setting of immunosuppression; the risk of developing non-melanoma skin cancers is of concern. Treatment options vary considerably, but often the lesions will recur upon cessation of therapy.
History
A 56-year-old man initially presented to the Dermatology Clinic at Bellevue Hospital Center in July, 2007, with thin hypopigmented and thin papules on the arms and legs since 2002. The patient's primary care physician was concerned about cancer and referred the patient to our clinic. Prior treatments prescribed by an outside dermatologist included topical 5-fluorouracil, ketconazole cream, clobetasol cream, and mometasone cream. Each topical therapy involved a two-month course. A punch biopsy was performed on the right leg.
 |  |
| Figure 1 | Figure 2 |
|---|
The patient has a history of human immunodeficiency virus infection for over 25 years, hypertension, and herpes simplex virus infection. He is taking a combination of lopinavir and ritonavir, nevirapine, tenofovir, acyclovir, diazide, atorvastatin, and fenofibrate. He is allergic to efavirenz.
Physical Examination
Hypopigmented, thin, pink, flat-topped papules coalescent to plaques were present on the chest, abdomen, back, arms, and legs. A fine scale was noted that became more prominent when the lesions were rubbed. A potassium hydroxide preparation of the scale showed no fungal elements. Lipoatrophy of the cheeks was also noted as were verrucous plaques on the back.
Lab
The white cell count was 6.2 x 109g/L, hematocrit 36 percent, platelet count 246 x 109g/L, lactate dehydrogenase 155 U/L, testosterone 275.22 ng/dL, Toxoplasma gondii antibody IgG negative, urine Chlamydia DNA negative, GC DNA negative, lipid profile normal, erythrocyte sedimentation 8 mm/hr, alkaline phosphatase 51 U/L, ALT 41U/L, basic metabolic panel normal, urinalysis: bilirubin 1+, trace leukocyte esterase, white cells 2 to 5, few bacteria, calcium oxalate crystals, HIV viral load 1850 copies/ml, and CD4 count 245 cells/mm³.
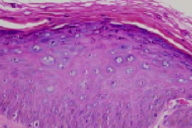
Histopathology
There is epidermal hyperplasia with hyperkeratosis, focal parakeratosis, and numerous, large keratinocytes with abundant blue-gray cytoplasm and keratohyaline granules in the upper spinous and granular layers.
Comment
Epidermodysplasia verruciformis (EDV) is normally an autosomal recessive disorder that may involve mutations in EVER1 and EVER2 genes that encode integral membrane proteins of the endoplasmic reticulum [1]. The disorder leads to a susceptibility to infections by multiple human papilloma virus (HPV) types, some of which are called EDV types. Widespread colonization by multiple HPV types and persistence of planar warts is noted in these patients [2]. The disease usually manifests in childhood, with lesions resembling flat warts or pityriasis versicolor. Frequently patients will also develop squamous-cell carcinomas, usually with HPV types 5 and 8. Sun exposure may increase risk of developing malignancies [2].
In the setting of immunosuppression, such as occurs with organ transplant recipients on immunosuppressive therapy, AIDS, and lymphoma, an EDV-like eruption can also develop. Several case reports of HIV-infected patients with EDV-like eruption have been described [3-8]. The EDV-type HPV can also be found in immunosuppressed patients [9]. The clinical features and histopathologic findings of EDV-like eruptions in the setting of immunosuppression resemble the inherited form, but in some cases the histology shows more dysplasia than does the inherited form [9]. Interestingly, EDV-type HPV have also been found in the normal skin of immunocompetent individuals who presumably act as reservoirs for susceptible individuals.
Treatment options vary considerably. In the inherited form, oral cimetidine therapy for three months reduced the extent of the lesions, with no relapse at six-month follow-up [10]. Photodynamic therapy with 5-aminolevulinic acid can also lead to histologic cure of active lesions with excellent cosmesis, but new lesions can develop [11]. A combination of acitretin and interferon alfa-2a has been helpful in one case study [12], whereas in another patient with EDV and multiple oral and genital mucosal squamous-cell carcinomas, acitretin with pegylated interferon alfa-2b for one year resulted in improvement of the warty lesions and no recurrence of mucosal cancer [13]. However, when interferon therapy was stopped, Bowen disease developed in the perianal region. In HIV infection, antiretroviral therapy (HAART) can induce remission [14], but the lesions can still remain despite HAART [15]. One case report described the development of EDV-like eruption after initiating HAART in an HIV-infected patient. This event was considered to be part of an immune restoration syndrome [16].
References
1. Ramoz N, et al. Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat Genet 2002; 32: 579 PubMed2. Majewski S, Jablonska S. Why epidermodysplasia verruciformis - a rare genetic disease - has raised such great interest. Int J Dermatol 2004; 43: 309 PubMed
3. Barzegar C, et al. Epidermodysplasia verruciformis-like eruption complicating human immunodeficiency virus infection. Br J Dermatol 1998; 139: 122 PubMed
4. Berger TG, et al. Epidermodysplasia verruciformis-associated papillomavirus infection complicating human immunodeficiency virus disease. Br J Dermatol 1991; 124: 79 PubMed
5. Davison SC, et al. Epidermodysplasia verruciformis-like eruption associated with HIV infection. Clin Exp Dermatol 2004; 29: 311 PubMed
6. Hu W, et al. Epidermodysplasia verruciformis in two half brothers with HIV infection. J Cutan Med Surg 2004; 8: 357 PubMed
7. Hultgren TL, et al. Epidermodysplasia verruciformis occurring in a patient with human immunodeficiency virus: a case report. Cutis 2007; 79: 307 PubMed
8. Prose NS, et al. Widespread flat warts associated with human papillomavirus type 5: a cutaneous manifestation of human immunodeficiency virus infection. J Am Acad Dermatol 1990; 23: 978 PubMed
9. Morrison C, et al. The histologic spectrum of epidermodysplasia verruciformis in transplant and AIDS patients. J Cutan Pathol 2002; 29: 480 PubMed
10. Micali G, et al. Cimetidine therapy for epidermodysplasia verruciformis. J Am Acad Dermatol 2003; 48: S9 PubMed
11. Karrer S, et al. Epidermodysplasia verruciformis treated using topical 5-aminolaevulinic acid photodynamic therapy. Br J Dermatol 1999; 140: 935 PubMed
12. Anadolu R, et al. Treatment of epidermodysplasia verruciformis with a combination of acitretin and interferon alfa-2a. J Am Acad Dermatol 2001; 45: 296 PubMed
13. Gubinelli E, et al. Epidermodysplasia verruciformis with multiple mucosal carcinomas treated with pegylated interferon alfa and acitretin. J Dermatolog Treat 2003; 14: 184 PubMed
14. Haas N, et al. Remission of epidermodysplasia verruciformis-like skin eruption after highly active antiretroviral therapy in a human immunodeficiency virus-positive patient. Br J Dermatol 2001; 145: 669 PubMed
15. Carre D, et al. Epidermodysplasia verruciformis in a patient with HIV infection: no response to highly active antiretroviral therapy. Int J Dermatol 2003; 42: 296 PubMed
16. Mermet I, et al. Cervical intraepithelial neoplasia associated with epidermodysplasia verruciformis HPV in an HIV-infected patient: a manifestation of immune restoration syndrome. Eur J Dermatol 2007; 17: 149 PubMed
© 2008 Dermatology Online Journal

