Post traumatic amelanotic subungual melanoma
Published Web Location
https://doi.org/10.5070/D34hf6j7j2Main Content
Post traumatic amelanotic subungual melanoma
Najet Ghariani MD, Lobna Boussofara MD, Nesrine Kenani, Nadia Ghannouchi, Amel Mebazaa MD, Mohamed Denguezli MD, Colandane
Belajouza MD, Rafia Nouira MD
Dermatology Online Journal 14 (1): 13
Department of Dermatology, Farhat Hached Hospital, 4002 SOUSSE, TUNISIAAbstract
Subungual melanomas are rare; a delay in the diagnosis is common and is associated with advanced stage. Part of the reason for a delay in presentation to the physician is that patients often attribute the lesion to trauma. Trauma may play a role in the pathogenesis or just draw attention to a skin tumor that may be more susceptible to injury. We report a case of subungual melanoma that was observed in an 86 year old man. The preceding trauma history and misleading clinical appearance delayed the diagnosis slightly. Biopsy of every nodular acral tumor is very important. A direct role of the trauma in the pathogenesis of melanoma remains unclear.
Subungual melanomas are rare, accounting for 2-3 percent of all cutaneous melanomas in the Caucasian population [1]. The great majority of subungual melanomas (90%) occur on the thumb or the great toe [2]. Delay in the diagnosis is common and is associated with an advanced stage. The role of preceding trauma in the pathogenesis of subungual melanoma has been suggested without being proven [3].
We report a case of subungual melanoma observed in an 86 year old man. The tumor was noted for a misleading clinical appearance and its noted onset after local trauma.
Clinical synopsis
 |
| Figure 1 |
|---|
| Figure 1. reddish, friable, broad-based nodule located on the tip of the fourth finger |
An 86-year-old man was seen in dermatology for a reddish nodule on his right fourth finger (Fig. 1). Initially, the patient noted rapid growth of the lesion over a period of one month following an injury made by nail clippers. Physical examination revealed a red, fleshy, friable nodule of one centimeter in diameter that bled easily.
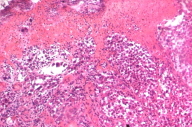
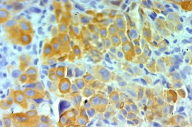
Histological study showed an epidermis that was largely ulcerated and a proliferation of large nucleated cells. These cells were isolated or gathered in irregular nests. The mitoses were numerous and the stroma was moderately inflammatory. The tumor cells reacted with the melanoma markers HMB 45 and melan A (Figs. 2, 3), confirming the melanoma diagnosis. There was no evidence of regional node involvement and screening for metastatic disease was negative. The patient has undergone a complete amputation of his fourth finger. Eight months later, multiple lung and liver metastases were detected and the patient died shortly thereafter.
 |  |
| Figure 2 | Figure 3 |
|---|---|
| Figure 2. Proliferation of melanoma cells isolated or gathered in nests(H&E x 200) Figure 3. Tumor cells reacted with the melanoma marker melan A | |
Discussion
Our patient had an amelanotic subungual melanoma. The differential diagnosis includes vascular tumors, especially pyogenic granuloma [4]. The latter is characterized by its bright red color, bleeding at the slightest touch, and rapid growth. Achromic melanoma may look very similar but generally has a slow, painless evolution that may last for months or years. Although we suspected pyogenic granuloma, the biopsy revealed the correct diagnosis. The notion of trauma preceding the appearance of a subungual melanoma has been reported in 23-24 percent of cases [1]. Some researchers suggest a direct role of trauma in the pathogenesis of melanoma [1]. Others object to this idea and believe that the trauma is just incidentally associated [5].
Conclusion
The diagnosis of subungual melanoma, in its achromic variant, is often delayed. This tumor must be differentiated from other subungual malignant or benign lesions, particularly pyogenic granuloma. Early biopsy of every nodular acral tumor is important. The direct role of trauma in the pathogenesis of sub-ungual melanoma remains unclear.
References
1. Mohrle M, Hafner H.M. Is subungual melanoma related to trauma? Dermatology. 2002;204(4):259-61. PubMed2. Blessing K, Kernohan NM, Park KG. Subungual malignant melanoma: clinicopathological features of 100 cases. Histopathology. 1991 Nov;19(5):425-9. PubMed
3. Kaskel P, Kind P, Sander S, Peter R.U, Krahn G. Trauma and melanoma formation: a true association? Br J Dermatol. 2000 Oct;143(4):749-53. PubMed
4. Harrington P, O'Kelly A, Trail IA, Freemont AJ. Amelanotic subungual melanoma mimicking pyogenic granuloma in the hand. J R Coll Surg Edinb. 2002 Aug;47(4):638-40. PubMed
5. O'Toole E.A, Stephens R, Young M.M, Tanner A, Barnes L. Subungual melanoma: a relation to direct injury? J Am Acad Dermatol 1995;Sep;33(3):525-8. PubMed
© 2008 Dermatology Online Journal

