Numerous fibrous papules of the face unassociated with any genodermatosis
Published Web Location
https://doi.org/10.5070/D30pc1r638Main Content
Numerous fibrous papules of the face unassociated with any genodermatosis
Jamie Elifritz MD1, Ravi S Krishnan MD2, Heidi Donnelly1
Dermatology Online Journal 13 (4): 12
1. Dayton Skin Surgery Center.e-mail:elifritz.3@wright.edu 2. :Department of Dermatology, Indiana University School of MedicineAbstract
Numerous angiofibromas on the face are commonly associated with tuberous sclerosis or multiple endocrine neoplasia type 1. We present a healthy 66-year-old female with numerous facial angiofibromas, without evidence of tuberous sclerosis, multiple endocrine neoplasia type 1, or any of the less common syndromes associated with many angiofibromas on the face. To our knowledge, there have been no previously reported cases of patients with numerous facial angiofibromas who did not have an associated genodermatosis.
Clinical synopsis
A 66-year-old healthy woman was referred to our practice for evaluation of multiple skin-colored papules on the face. The papules first appeared 50 years earlier. At the time the lesions had first appeared, the patient had been told by her dermatologist that the lesions were trichoepitheliomas. She had never had any skin biopsies, but some of the lesions were removed with curettage and light hyfrecation. She never applied any medications to her face with the exception of intermittent pimecrolimus cream, which her primary care physician had prescribed for occasional, mild pruritus that was associated with the lesions. On physical examination, she was noted to have approximately 100-150 1-10 millimeter skin-colored papules predominantly located on the cheeks, but also present on the nose, forehead, and cutaneous portion of the lip.
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Clinical photograph of patient with multiple fibrous papules | |
| Figure 2. Closer view | |
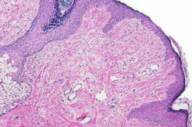
Biopsies were taken from four of the lesions for histopathologic examination. Representative findings can be seen in Fig. 3 and include fibrosis and an increased number of blood vessels in the upper dermis. Based on these findings, a diagnosis of angiofibroma was made.
 |
| Figure 3 |
|---|
| Figure 3. Photomicrograph showing histopathology of the lesions |
At this point, a more detailed history was obtained from the patient. Her only medical problems were osteoarthritis (for which she took acetaminophen) and mild gastroesophageal reflux (for which she took omeprazole). Also of note, the patient had a history of seizures 40-50 years prior to presentation, which were successfully treated with phenytoin. Since the onset of the seizures, the patient had multiple brain MRI studies, all of which were unremarkable. Furthermore, she has not had any further seizures or taken phenytoin for over 35 years.
The patient had no family history, signs, or symptoms of either tuberous sclerosis or endocrine disorders. She also denied having family members with skin lesions similar to hers. She had an entirely unremarkable neurological examination, and a full skin examination failed to reveal any stigmata of tuberous sclerosis, including ash-leaf macules, café-au-lait macules, shagreen patches, or periungual fibromas. She reported that all of her routine ophthalmologic and dental examinations had been normal. She also denied any symptoms associated with endocrine disorders, and a full endocrine work-up was unremarkable. Based on this lack of other findings which may be associated with multiple angiofibromas, we determined that this patient's angiofibromas were simply multiple fibrous papules and not associated with any syndrome.
Comment
Angiofibromas are common benign neoplasms. Classically, they appear as small, firm, discrete, skin-colored papules. They usually develop on the faces of adults. Generally, angiofibromas can be readily diagnosed on the basis of clinical and histologic criteria. There are four main clinical variants of angiofibromas: fibrous papules, adenoma sebaceum, Koenen tumors, and pearly penile papules [1]. These lesions are clinically distinct, yet histologically similar.
Fibrous papules on the face usually arise as single lesions; however, occasionally multiple (i.e., normally less than 10) lesions may be present [2]. Occurring predominantly on the nose, these lesions are generally 1-5 mm, shiny, skin-colored, firm, dome-shaped papules. The lesions observed on our patient were clinically most similar to fibrous papules.
Lesions of adenoma sebaceum are discrete, firm, reddish papules that frequently develop in the nasolabial folds during late childhood to early adolescence, increasing in size and number during puberty [3]. They are strongly associated with tuberous sclerosis. Koenen tumors are another clinical variant of angiofibromas that are associated with tuberous sclerosis [3]. Clinically presenting as subungual and periungual fibromas, Koenen tumors develop around the time of puberty and appear as firm, smooth, skin-colored papules 5-10 millimeters in diameter.
Pearly penile papules are another relatively common type of angiofibroma. They are small, dome-shaped to filiform, skin-colored papules situated circumferentially around the corona or sulcus of the penis. Pearly penile papules occur on approximately 10 percent of males, and they are more common on those who are uncircumcised [4].
The clinical differential diagnosis of angiofibromas includes adnexal tumors, such as trichoepitheliomas, and basal cell carcinoma. However, histopathologic examination of a lesion will readily distinguish angiofibromas from these other entities. Furthermore, when numerous and located on the face, angiofibromas are commonly associated with tuberous sclerosis [3] or multiple endocrine neoplasia type I [5, 6]. Therefore, in patients with multiple fibrous papules on the face, these other conditions should be excluded by thorough history-taking, comprehensive physical examination, and appropriate diagnostic testing.
There have been also rare reports of multiple fibrous papules in association with type-II neurofibromatosis [7], Cowden disease [8], Birt-Hogg-Dube syndrome [9], and Hornstein-Knickenberg syndrome, which some authors believe is a variant of Birt-Hogg-Dube syndrome [10, 11]. Our patient had no signs or symptoms of any of these syndromes. We offered the patient imaging studies to further investigate the possibility of Birt-Hogg-Dube syndrome, but she declined. However, because the patient has no affected family members and no other stigmata, we believe that a diagnosis of Birt-Hogg-Dube is unlikely.
Histologically, angiofibromas are characterized by a proliferation of numerous hyperplastic blood vessels with perivascular and periadnexal fibrosis [12]. This fibrous tissue often consists of stellate fibroblasts, some of which may be multinucleated [12]. Periodically, scattered lymphocytes and a sparse inflammatory cell infiltrate can be appreciated [2]. Numerous different histological subtypes of angiofibroma have been described [2, 12, 13]. These subtypes all share the aforementioned histologic features, which are found in all angiofibromas, but, in addition, each described subtype has a certain unique quality that renders it distinct.
Several options are available for the removal of fibrous papules. We routinely employ surgical procedures such as curettage, shave excision, or elliptical excision with excellent cosmetic results. Successful treatment with various lasers, including the pulsed dye laser [14, 15, 16, 17], CO2 laser [16, 17], KTP laser [18], and argon laser [17]. Our patient stated that the appearance of the lesions was of little concern to her, so she was not interested in treatment.
To our knowledge, this is the only reported case of a patient with so many angiofibromas on the face that are not associated with a genetic syndrome. We routinely encounter patients with solitary or even several fibrous papules on the face. The prodigious number of angiofibromas which our patient had is certainly far greater than that which is normally seen in patients with fibrous papules and suggested to us that they may be a part of a larger disease process. However, after a thorough evaluation, our patient demonstrated no evidence of a genodermatosis or other syndrome. Therefore, we feel that her lesions are simply multiple fibrous papules.
References
1. Meigel WN, Ackerman AB. Fibrous papule of the Face. Am J Dermatopathol. 1979 Winter;1(4):329-40. PubMed2. Bansal C, Stewart D, Li A, Cockerell CJ. Histologic variants of fibrous papule. J Cutan Pathol. 2005 Jul;32(6):424-8. PubMed
3. Barbagallo JS, Kolodzieh MS, Silverberg NB, Weinberg JM. Neurocutaneous disorders. Dermatol Clin. 2002 Jul;20(3):547-60, viii. PubMed
4. Glicksman JM, Freeman RG. Pearly penile papules. Arch Dermatol. 1966 Jan;93(1):56-9. PubMed
5. Schussheim DH, Skarulis MC, Agarwal SK, Simonds WF, Burns AL, Spiegel AM, Marx SJ. Multiple endocrine neoplasia type 1: new clinical and basic findings. Trends Endocrinol Metab. 2001 May-Jun;12(4):173-8. PubMed
6. Darling TN, Skarulis MC, Steinberg SM, Marx SJ, Spiegel AM, Turner M. Multiple facial angiofibromas and collagenomas in patients with multiple endocrine neoplasia type 1. Arch Dermatol. 1997 Jul;133(7):853-7. PubMed
7. Jaffe AT, Heymann WR, Schnur RE. Clustered angiofibromas on the ear of a patient with neurofibromatosis type 2. Arch Dermatol. 1998 Jun;134(6):760-1. PubMed
8. Yamamoto T, Katayama I, Nishioka K. Fibropapule multiplex of the nose: a variant of Cowden's disease? Dermatology. 1996;192(4):379-81. PubMed
9. Schaffer JV, Gohara MA, McNiff JM, Aasi SZ, Dvoretzky I. Multiple facial angiofibromas: a cutaneous manifestation of Birt-Hogg-Dube syndrome. J Am Acad Dermatol. 2005 Aug;53(2 Suppl 1):S108-11. PubMed
10. Schulz T, Hartschuh W. Birt-Hogg-Dube syndrome and Hornstein-Knickenberg syndrome are the same. Different sectioning technique as the cause of different histology. J Cutan Pathol. 1999 Jan;26(1):55-61. PubMed
11. Schulz T, Hartschuh W. Characteristics of the Birt-Hogg-Dube/Hornstein-Knickenberg syndrome. Am J Dermatopathol. 2000 Jun;22(3):293-4. PubMed
12. Requena L, Sangueza OP. Cutaneous vascular proliferations. Part III. Malignant neoplasms, other cutaneous neoplasms with significant vascular component, and disorders erroneously considered as vascular neoplasms. J Am Acad Dermatol. 1998 Feb;38(2 Pt 1):143-75; quiz 176-8. PubMed
13. Guitart J, Bergfeld WF, Tuthill RJ. Fibrous papule of the nose with granular cells: two cases. J Cutan Pathol. 1991 Aug;18(4):284-7. PubMed
14. Sharma VK, Khandpur S, Khanna N. An interesting case of unilateral angiofibromas successfully treated with pulsed dye laser. J Eur Acad Dermatol Venereol. 2004 Sep;18(5):641-2. PubMed
15. Paquet P, Hermans JF, Pierard GE. Effect of the 585 nm flashlamp-pumped pulsed dye laser for treatment of keloids. Dermatol Surg. 2001 Feb;27(2):171-4. PubMed
16. Papadavid E, Markey A, Bellaney G, Walker NP. Carbon dioxide and pulsed dye laser treatment of angiofibromas in 29 patients with tuberous sclerosis. Br J Dermatol. 2002 Aug;147(2):337-42. PubMed
17. Boixeda P, Sanchez-Miralles E, Azana JM, Arrazola JM, Moreno R, Ledo A. CO2, argon, and pulsed dye laser treatment of angiofibromas. J Dermatol Surg Oncol. 1994 Dec;20(12):808-12. PubMed
18. Tope WD, Kageyama N. "Hot" KTP-laser treatment of facial angiofibromata. Lasers Surg Med. 2001;29(1):78-81. PubMed
© 2007 Dermatology Online Journal

