An infant with bullous pemphigoid
Published Web Location
https://doi.org/10.5070/D33pq8v0b8Main Content
An infant with bullous pemphigoid
António Luís Santos MD1, Alberto Vieira Mota PhD1, José Ramon MD2, José Manuel Lopes PhD2, Filomena Azevedo MD1
Dermatology Online Journal 13 (3): 17
1.Dermatology Department, Hospital de São João and Faculty of Medicine of Oporto, Portugal2. Pathology Department, Hospital de São João and Faculdade de Medicina do Porto
Abstract
Bullous pemphigoid is the most common subepidermal autoimmune blistering disease. However, it is very rare in the pediatric population. A 5-month-old male infant presented with multiple bullae located on palms and soles. Complete blood count revealed relative eosinophilia . A biopsy revealed a subepidermal blister present along with a dermal mononuclear infiltrate rich in eosinophils. In focal areas colagen flame figures, were also observed. Direct immunofluorescence showed linear reactivity for C3c and IgG at the dermal-epidermal junction. IgA was not found. Complete resolution was achieved after oral deflazacort (1.5mg/kg/day) with progressive dose reduction over 2 weeks. Bullous pemphigoid is extremely rare in the infant. In our case the disease presented with an unusual localized (acral) clinical distribution and a favorable outcome.
Bullous pemphigoid (BP) is an acquired autoimmune subepidermal blistering disease very rare in the pediatric population [1]. This report describes a case of BP in a 5-month-old infant who had an acral distribution of the lesions and a rapid response to treatment.
Clinical synopsis
A 5-month-old male infant presented with multiple large, tense bullae on an erythematous base, filled with clear fluid. The bullae were located predominantly on palms and soles (Fig. 1). The eruption had started a week before and spared the mucous membranes. The infant was previously well without systemic signs, including fever. There was no relevant problems during gestation and delivery. He was exclusively breastfed.
 |  |
| Figure 1 | Figure 2 |
|---|---|
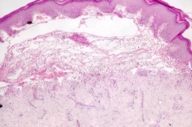
| Figure 1. Multiple bullous lesions in soles Figure 2. Subepidermal blister with dermal inflammatory infiltrate (H&E; 20X) | |
 |  |
| Figure 3 | Figure 4 |
|---|---|
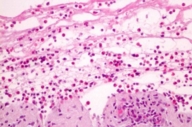
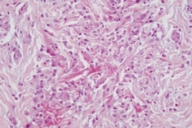
| Figure 3. Dermal inflammatory infiltrate rich in eosinophils (H&E; 40X) Figure 4. Flame figures in dermis (H&E; 100X) | |
Complete blood count revealed relative eosinophilia (17.2 %; WBC 15.6x109/L). Sedimentation rate was slightly elevated. The bacteriological exam of the blister fluid, the serological markers for HSV 1 and 2, and the titers of anti-basement membrane IgG were negative; syphilis serology was also negative.
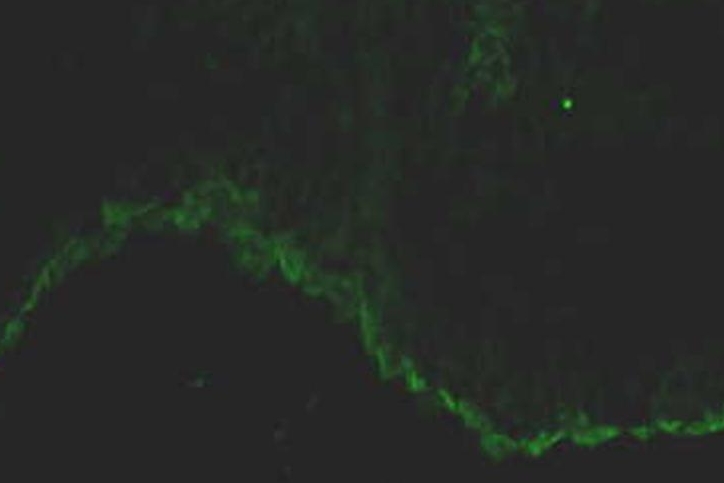
Upon histopathological examination, a subepidermal blister was present along with a dermal leucocyte infiltrate rich in eosinophils (Figs. 2 and 3). In focal areas, collagen flame figures were also observed (Fig. 4). On direct immunofluorescence, linear reactivity for C3c and IgG was found at the dermal-epidermal junction (Fig. 5). There was no IgA immunostaining present.
 |  |
| Figure 5 | Figure 6 |
|---|---|
| Figure 5. Linear deposition of IgG in basement membrane in direct immunofluorescence. Figure 6. Clinical aspect 1 week after starting oral treatment. | |
After topical glucocorticoid therapy, complete resolution without scarring was achieved. However, recurrence occurred after 2 weeks. It was then decided to begin treatment with oral deflazacort (1.5mg/kg/day) with progressive dose reduction over 2 weeks (Fig. 6). The child is now free of lesions for 1 year.
Discussion
Bullous pemphigoid is an immune-mediated disease that is associated with a humoral and cellular response directed against two well-characterized self-antigens: BP antigen 180 and BP antigen 230 [1, 2].
In some children, the clinical features of BP may be indistinguishable from those of adult disease. However, in childhood BP, the lesions are often localized rather than widespread and acral distribution is more common. More often the disease is self-limited and responds well to topical or systemic steroids. Some previous reports have emphasized that BP in infants initially presents on the palms and soles [2, 3]. In our patient the lesions were predominantly in this location without further spreading.
Histologically, childhood BP is characterized by eosinophil-rich subepidermal blisters indistinguishable from adult disease [1, 3]. In our patient, besides these typical findings, flame figures were present in the dermis, a pattern rarely described in BP. This finding results from the adherence of amorphous or granular eosinophilic material to collagen bundles in the dermis [4].
In almost all patients direct IF microscopy studies of perilesional, uninvolved skin characteristically demonstrate the presence of fine, linear, continuous deposits of IgG and/or C3 along the basement membrane, as was the case in our patient [1, 2, 3]. The main differential diagnostic is inflammatory epidermolysis bullosa acquisita (EBA) [5]. Because our patient’s localized inflammatory subepidermal blistering disease was not associated with trauma and he had an excellent and prolonged therapeutic response with no scarring, EBA would be highly unlikely.
Childhood BP usually follows a self-limited course with appropriate therapy, including topical or oral corticosteroids. With most patients, remission is achieved within the first year [1]. In our patient the response to topical steroids was quite good. However, after suspension the lesions recurred and only after introduction of oral deflazacort the remission was sustained.
This report illustrates the importance of considering a diagnosis of BP in any child or infant who presents with blisters of the hands and feet, and performing the necessary immunofluorescence studies to make a definitive diagnosis [1, 2, 3].
References
1. Fisler RE, Saeb M, Liang MG, Howard RM, McKee PH. Childhood bullous pemphigoid: a clinicopathologic study and review of the literature. Am J Dermatopathol. 2003 Jun;25(3):183-9. PubMed2. Amos B, Deng JS, Flynn K, Suarez S. Bullous pemphigoid in infancy: case report and literature review. Pediatr Dermatol. 1998 Mar-Apr;15(2):108-11. Dermatol 1998 May-Jun;15(3):202. PubMed
3. Nemeth AJ, Klein AD, Gould EW, Schachner LA. Childhood bullous pemphigoid. Clinical and immunologic features, treatment, and prognosis. Arch Dermatol. 1991 Mar;127(3):378-86. PubMed
4. Weedon D. An approach to the interpretation of skin biopsies. In Weedon D (Ed), Skin Pathology, 1st ed, Churchill Livingstone, 1998, pp 3-14.
5. Edwards S, Wakelin SH, Wojnarowska F, Marsden RA, Kirtschig G, Bhogal B, Black MM. Bullous pemphigoid and epidermolysis bullosa acquisita: presentation,prognosis, and immunopathology in 11 children. Pediatr Dermatol. 1998 May-Jun;15(3):184-90. PubMed
© 2007 Dermatology Online Journal

