Primary epidermoid carcinoma of the submandibular salivary gland
Published Web Location
https://doi.org/10.5070/D37p46v3q7Main Content
Primary epidermoid carcinoma of the submandibular salivary gland
A Elloumi-Jellouli, F Derbel1, M Jellouli2, S Ben Ammar, K Mrad3, Kh Ben Romdhane3
Dermatology Online Journal 11 (1): 26
Ettadhamen Hosptal, Ariana Tunisia1. FSI Hospital, La Marsa 2. Oral And Cervico-Facial Surgery Department, Menzel Bourguiba
Hospital. amel.jellouli@laposte.net 3. Anatomopathology Department, Salah Azaiz Institut
Clinical synopsis
A 65-year-old man with a history of alcoholism and smoking (60 pack-year), was admitted for exploration of a left submandibular tumefaction of one year's duration. There were no similar cases in the family and no history of contact with tuberculosis. There was no history of surgical or radiological intervention in the submandibular region.
Physical examination revealed a 4 × 3-cm firm, painless tumor of submandibular region; it was fixed to superficial and deep planes. The patient had poor dentition. Laryngoscopic examination was normal. Ultrasound revealed the presence of a relatively well-demarcated submandibular tumor with a central necrotic area. The radiography of the chest was normal.
An excision was scheduled, but the patient failed to show.
He finally returned 2 months later, the tumor having greatly enlarged. Multiple nodules were present under erythematous, indurated skin involving the left submandibular region, the chinstrap region, and the upper neck (Fig. 1). The facial nerve appeared to be involved because there was drooping of the lower lip and paresis of the chin.

|
|
| Figure 1 | Figure 2 |
|---|---|
| Multiple nodules under inflamed skin (Fig. 1). | |
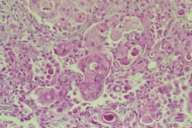
| Epidermoid carcinoma of the submandibular gland (H&E × 400) (Fig. 2). | |
Comment
The clinical diagnosis was primary epidermoid carcinoma of the submandibular salivary gland. Ultrasound demonstrated diffuse tumor formation in the submandibular gland and identified lymphadenopathy. Once the diagnosis was confirmed by frozen section, the patient underwent wide excision and a lymph-node dissection. Pathology examination of the surgical specimen revealed irregular masses and cords of epithelial cells invading the submandibular gland, along with large nuclei and many mitotic figures (Fig. 2). The tumor stained negative for mucous. The overlying skin was intact and not involved. The diagnosis was undifferentiated carcinoma of the submandubular gland.
Most pathology involving the submandibular gland is inflammatory. In ninety percent of specimens, the diagnosis is sialolithiasis. Cellulitis or chronic adenopathy is usually due to tuberculosis [1]. Both of these diagnoses were easily eliminated in our patient. Tumors of a salivary gland more often occur in the parotid rather than the submandibular gland, but those that occur in the submandublar gland are more often malignant.
Primary epidermoid carcinoma of major salivary glands is rare. The major risk factor is a history of radiotherapy of this gland, not experienced by our patient [1, 2, 3]. It is important to rule out a metastasis of an epidermoid carcinoma from elsewhere on the head and the neck, or (rarely) metastasis from visceral cancer, such as lung cancer [4, 5].
Patients with spinocellular carcinoma of major salivary glands are predominantly male. Clinically, they present with an asymptomatic, poorly encapsulated, nodular tumor. It is fixed to superficial and deep planes. The invasion of the facial nerve or one of its branches is possible, but rare [1].
Radical excision with preservation of the facial nerve when possible is the treatment of choice. Radical neck dissections are not uniformly employed. Adjunctive treatment with radiotherapy or chemotherapy is recommended. Local or regional recurrence occurs in both parotid (51 %) and submandibular (67 %) cases [3].
Prognosis is strongly correlated with the stage of the tumor. The 5-year survival usually varies from 50 to 80 percent, but for end-stage disease does not exceed 14 percent [3, 6, 7].
Conclusion
This patient was interesting because of the rarity of the primary epidermoid carcinoma of the submandibular gland, the involvement of the facial nerve, and the advanced stage.
References
Taxy JB. Squamous carcinoma in a major salivary gland: a review of the diagnostic considerations. Arch Pathol Lab Med. 2001 Jun;125(6):740-5. PubMed2. Li J, Wang BY, Nelson M, Li L, Hu Y, Urken ML, Brandwein-Gensler M. Salivary adenocarcinoma, not otherwise specified: a collection of orphans. Arch Pathol Lab Med. 2004 Dec;128(12):1385-94. PubMed
3. Shemen LJ, Huvos AG, Spiro RH. Squamous cell carcinoma of salivary gland origin. Head Neck Surg. 1987 Mar-Apr;9(4):235-40. PubMed
4. Seifert G, Hennings K, Caselitz J. Metastatic tumors to thr parotid and submandibular glands--analysis and differential diagnosis of 108 cases. Pathol Res Pract 1986 Dec;181(6):684-692. PubMed
5. Nichols RD, Pinnock LA, Szymanowski RT. Metastases to parotid nodes. to the Laryngoscope 1980;90:1324-8. PubMed
6. Andersen LJ, Therkildsen MH, Ockelmann HH, Bentzen JD, Schiodt T, Hansen HS. Malignantepithelial tumors in the minor salivary glands, the submandibular gland and the sublingual gland: prognostic factors and treatment results. Cancer 1991; 68(11):2431-2437. PubMed
7. Spiro RH, Armstrong J, Harrison L, Geller NL, Lin SY, Strong EW. Carcinoma of major salivary glands. Recent trends. Arch Otolaryngol Head Neck Surg. 1989 Mar;115(3):316-21.PubMed
© 2005 Dermatology Online Journal

