Telangiectasia macularis eruptiva perstans
Published Web Location
https://doi.org/10.5070/D30gp977bvMain Content
Telangiectasia macularis eruptiva perstans
Nathalie Q Nguyen MD
Dermatology Online Journal 10 (3): 1
From the Ronald O. Perelman Department of Dermatology, New York University
Abstract
A 45-year-old man presented with lesions clinically and histologically consistent with telangiectasis macularis eruptiva perstans (TMEP). TMEP is a rare form of mastocytosis, which is localized to the skin, although systemic involvement has been reported. A mutation in the c-kit proto-oncogene is thought to be involved in mast cell hyperplasia in some patients with mastocytosis. Treatment depends on the presence of systemic involvement or clinical symptoms. In case reports, therapeutic benefit has been reported in TMEP with the use of the 585-flashlamp pumped dye lasers and of electron beam radiation.
Clinical summary
History.—A 45-year-old man with a history of hypertension presented to the New York Harborview Health Care System with red-tan spots on his chest and back. He stated that they had not been present during childhood but developed over the past five to ten years. He denied itching or burning. There were no systemic features. He did not have any family members with similar skin lesions.
Physical Examination.— Multiple, red-tan macules with telangiectases were scattered on the chest, shoulders, and back. The lesions blanched with diascopy but did not urticate, blister, or itch after a brisk stroke. There was no hepatosplenomegaly or lymphadenopathy.

|
|
| Figure 1 | Figure 2 |
|---|
Laboratory data.— Liver function tests, a basic metabolic panel, and a complete blood count were normal.
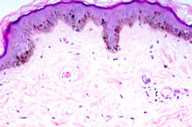
Histopathology.— There is an increased number of mast cells around the dilated thin-walled blood vessels in the papillary dermis. There is some increased pigmentation of the epidermal basal layer.
Diagnosis.—Telangiectasia macularis eruptiva perstans.
Comment
Telangiectasia macularis eruptiva perstans (TMEP), which was described by Parkes Weber in the 1930s, represents a rare form of mastocytosis [1]. The lesions typically consist of telangiectatic macules and have a background color ranging from tan to brown. TMEP typically develops in adults, although there have been case reports of TMEP in children.
Familial TMEP has been reported in four children in three generations of one family [2]. Traditionally, TMEP has been thought to be a form of mastocytosis limited to the skin; however, patients may also report signs of systemic involvement that include headaches, flushing, diarrhea, splenomegaly, abnormal skeletal radiographs, and bone-marrow involvement [3].
Mastocytosis is characterized by an increase in the number of mast cells in one or more organs. A mutation in the c-kit proto-oncogene results in mast-cell hyperplasia [4]. The c-kit proto-oncogene encodes KIT, a tyrosine kinase, which is the receptor for mast-cell growth factor. In a study of adult patients with sporadic mastocytosis, a somatic c-kit mutation in codon 816 led to spontaneous activation of the mast-cell growth-factor receptor. This specific mutation, however, was not found in pediatric patients or familial cases of mastocytosis.
Although mutations in c-kit are not found in all patients with cutaneous mastocystosis, alterations in this proto-oncogene may indicate more aggressive mastocytosis [5]. Studies of c-kit have not been performed in TMEP.
Although TMEP is a cutaneous manifestation of mastocytosis, systemic involvement may occur. Elevated serum tryptase levels may serve as a guide for systemic involvement [6]. In a study of 52 patients, the prevalence of bone-marrow biopsy specimens that indicated systemic mastocytosis increased as the level of total tryptase increased. The biopsy specimens were 100 percent positive when total tryptase was greater than 75 ng/ml and 50 percent positive when total tryptase levels were 20-75 ng/ml.
Treatment of patients with TMEP depends on the presence of systemic involvement or clinical symptoms. For those patients with cutaneous lesions only, management remains symptomatic with antihistamines and the avoidance of ingestants known to stimulate mast-cell degranulation. The use of the 585-nm flashlamp-pumped dye laser in two patients and of total electron beam radiation in one patient has been of benefit in treatment of the cutaneous lesions [7, 8].
References
1. Soter NA. Mastocytosis and the skin. Hematol Oncol Clin North Am 2000; 14:537.2. Chang A, et al. Familial cutaneous mastocytosis. Pediatr Dermatol 2001;18:271.
3. Tebbe B, et al. Cutaneous mastocytosis in adults. Dermatology 1998;197:101.
4. Longley BJ, et al. Activating and dominant inactivating c-kit catalytic domain mutations in distinct clinical forms of human mastocytosis. Proc Natl Acad Sci (USA) 1999; 96:1609.
5. Longley BJ, et al. Somatic c-kit activating mutations in urticaria pigmentosa and aggressive mastocytosis: establishment of clonality in a human mast cell neoplasm. Nat Genet 1996; 12:312.
6. Schwartz LB, et al. Serum tryptase and the laboratory diagnosis of systemic mastocytosis. Hematol Oncol North Am 2000; 14:641.
7. Monahan TP, et al. Treatment of telangiectasia macularis eruptiva perstans with total skin electron beam radiation. Cutis 2003; 71:357.
8. Ellis DL. Treatment of telangiectasia macularis eruptiva perstans with the 585-nm flashlamp-pumped dye laser. Dermatol Surg 1996; 22:33.
© 2004 Dermatology Online Journal

