Papulonodular mucinosis with subacute cutaneous lupus erythematosus
Published Web Location
https://doi.org/10.5070/D32pc672ktMain Content
Papulonodular mucinosis with subacute cutaneous lupus erythematosus
Carole Hazan MD
Dermatology Online Journal 10 (3): 6
From the Ronald O. Perelman Department of Dermatology, New York University
Abstract
A 30-year-old woman with subacute cutaneous lupus erythematosus presented with a facial eruption, painful and swollen ulcers of her digits, and asymptomatic lesions on her abdomen. The laboratory findings were consistent with subacute cutaneous lupus erythematosus with an anticardiolipin antibody. A biopsy specimen of the asymptomatic lesions on her abdomen showed mucin within the upper reticular dermis. Papulonodular mucinosis is a rare but wel-documented finding associated with systemic and cutaneous forms of lupus erythematosus. The etiology and pathogenesis of this finding remain to be elucidated.
History.—A 31-year-old woman presented with a 1-month history of a rash on the face, arms, chest, and abdomen. The patient presented to the Bellevue Hospital Medical Center Dermatology Clinic with a 1-year history of rheumatoid arthritis and two miscarriages. She was maintained on prednisone when she presented with a facial eruption, painful swelling, ulcers of her digits, and asymptomatic lesions on her abdomen. She was otherwise well, with no other systemic complaints.
Physical Examination.—Erythematous patches were noted on the nasolabial folds, eyebrows, and medial aspects of the cheeks. The volar aspects of her digits had erythematous and white, atrophic plaques with superficial ulcers. Multiple, dome-shaped, yellow, translucent papules were noted in an asymmetric distribution on her abdomen. Confluent erythematous plaques with excoriations were present on her arms and upper chest in a sun-exposed distribution.

|
|
| Figure 1 | Figure 2 |
|---|
Laboratory Data.—The complete blood cell count with differential analysis, erythrocyte sedimentation rate, blood chemistry profile, and urinalysis was normal. Nuclear antibody SS-A was positive at 11.8 U/ml. The antinuclear antibody titer was 1:320. Double-stranded DNA antibody was positive at a value greater than 200 IU/ml. The anti-SM antibody was positive 1.01, and anti-RNP antibody was positive at greater than 6 (with a range greater or equal to 1.0). The anti cardiolipin IgG was positive at 28 (with a range from 1-9). IgG phospholipids unit and the IgM were normal.
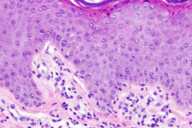
Histopathology.—There is increased connective-tissue mucin within the upper reticular dermis.
Diagnosis.—Papulonodular mucinosis with subacute cutaneous lupus erythematosus.
Comment
Cutaneous mucinoses are a heterogeneous group of diseases in which mucin accumulates in the dermis or within hair follicles. They can be divided into two groups: (1) those in which the mucin deposition is a distinctive histopathologic feature that is manifested as a clinically specific lesion; and (2) those associated with diseases with histopathologic mucin deposition as an additional finding. Papular and nodular mucinosis associated with either systemic or cutaneous lupus erythematosus (LE) is a rare condition with less than 40 cases documented to date. They have been reported either as part of the skin findings in SLE or as an isolated cutaneous form of LE. Red-purple to skin-colored papules and nodules, and in extreme cases plaques, are often present on the trunk, arm, head, and neck. Histopathologically, there are abundant mucin deposits in the dermis without the microscopic features of LE. Although mucin deposition is a common finding in LE, it is rarely present in sufficient quantity to produce clinically visible lesions.
The etiology and pathogenesis are still unknown. The documented cases have highlighted possible associations with the onset of PUVA photochemotherapy and immunosuppressive therapy with prednisone [1, 2]. One study has postulated a mechanism in which the production of glycosaminoglycans by dermal fibroblasts is increased and thought to be stimulated by a factor (or factors) in the patient's serum that are as yet unidentified [3]. Underlying vasculopathies or vascular changes are thought to be closely related to the mucin deposition [4, 5].
References
1. Terao H, et al. A case of nodular cutaneous lupus mucinosis. J Dermatol 2003;30:341.2. Nishimoto M., et al. Cutaneous mucinosis associated with SLE: a case provoked by PUVA. J Dermatol 1989;16:374.
3. Pandya AG, et al. Papulonodular mucinosis associated with systemic lupus erythematosus: possible mechanisms of increased glycosaminoglycan accumulation. J Am Acad Dermatol 1995;32:199.
4. Kanda N, et al. Cutaneous lupus mucinosis: a review of our cases and the possible pathogenesis. J Cutan Pathol 1997;24:553.
5. Egawa H, et al. Nodular cutaneous lupus mucinosis associated with atrophie blanche-like lesions in a patient with systemic lupus erythematosus. J Dermatol 1994;21:674.
© 2004 Dermatology Online Journal

